Comparative Study on the Effect of Parity on Serum Bone Mineralization Parameters (Calcium and Phosphate) in Pre- and Post-Menopausal Women
1Faculty of Basic Medical Sciences, Department of Physiology, College of Medicine, Ambrose Alli University Ekpoma
2Department of Basic/Allied Medical Sciences, College of Medical Sciences, Edo University, Iyamho
- *Corresponding Author:
- Ekhator CN
Faculty of Basic Medical Sciences
Department of Physiology, College
of Medicine, Ambrose Alli University Ekpoma, Nigeria
Tel: +2348032770151
E-mail: clemo4real@yahoo.co.uk
Received Date: February 18, 2018 Accepted Date: May 30, 2018 Published Date: June 05, 2018
Citation: Ekhator CN, Ebomoyi MI (2018) Comparative Study on the Effect of Parity on Serum Bone Mineralization Parameters (Calcium and Phosphate) in Pre- and Post- Menopausal Women. J Women’s Health Reprod Med. Vol.2 No.1:4
Abstract
The objective of this study was to evaluate and compare serum calcium and phosphate status in pre-menopausal and postmenopausal women and determine the effect of parity in postmenopausal women. The study was a cross sectional study was carried out in a catholic mission hospital in Benin City, Nigeria. A total of 40 pre-menopausal and 280 post postmenopausal women with 40 each with parity ranging from 0 to 6 were included in this study. Following standard ethical process and laboratory procedures blood sample was obtained from each woman for estimation of serum calcium and phosphate concentrations. Statistical analysis was done using SPSS version 20 and the student t test and ANOVA carried out for statistical different at 95% confidence interval. The result showed that serum calcium (11.07 ± 1.53 mg/dl vs. 8.20 ± 0.41 mg/dl; 25.93% deficient) was significantly reduced while serum phosphate (2.39 ± 0.45 mg/dl vs. 3.71 ± 0.71 mg/dl; 55.23% surfeit) was significantly increased in postmenopausal women compared to the premenopausal women values. Compared to nulliparous postmenopausal women (8.11 ± 0.39 mg/dl), postmenopausal women in their 1st (8.49 ± 0.39 mg/dl) and 2nd (8.64 ± 0.31 mg/dl) parities have significantly higher mean serum calcium level while those in their 3rd through 6th parity have nonsignificantly lower mean serum calcium level. On the other hand, compared to the nulliparous postmenopausal women (2.66 ± 0.09 mg/dl), mean serum phosphate levels were significantly higher in irrespective of the number of parities.
Keywords
Parity; Postmenopausal; Calcium; Phosphate
Introduction
Menopause is the permanent cessation of menstruation, seen in women between 40 to 61 years of age and characterized by the menstrual changes that reflect oocyte depletion and subsequent reduction in ovarian hormone production [1]. Due to menopause ovarian follicles loss its function, which results in decreased production of estradiol and other hormones [2]. Decreased levels of estrogen leads to increased osteoclast formation and enhanced bone resorption, which intern leads to loss of bone density and destruction of local architecture resulting in osteoporosis [3]. After age 40-50, bone loss may progress slowly in both sexes, with a period of more rapid loss in women surrounding the menopausal transition [4] and this leads to osteoporosis.
Osteoporosis is a metabolic bone disorder characterized by a decrease in bone strength and an increase in bone fragility [5]. Genetic, hormonal and environmental factors contribute to osteoporosis development [6-8]. The effects of multiparity on the bone mineral density in the post-menopausal period are still controversial. While some researchers report an absence of a positive or negative effect of parity on bone mineral density [9,10], there are others who have reported a positive effect [11] or a negative effect on bone mineral density [12,13].
It is known that several changes occur during pregnancy and lactation and that these changes can affect bone mass, including changes in reproductive hormones and in hormones that affect calcium metabolism. For example, intestinal calcium absorption increases during pregnancy to meet many of the fetal calcium needs, but maternal bone losses may occur in the last months of pregnancy [14]. The mother’s skeleton also loses bone during breastfeeding, but this loss is largely restored during weaning, as ovulation and menses are re-established [15]. This bone loss and its subsequent restoration appear to be independent of lifestyle behaviors, including dietary calcium intake and physical activity patterns [16]. In this regard, Bayray and Enquselassie [15] were of the view that since fetal and infant bone growth during pregnancy and lactation depends on calcium transfer from the mother, thus the possibility that pregnancy and lactation may influence the risk for bone mineral loss later in life. With this background, this study was conducted to estimate and compare serum calcium and phosphate in postmenopausal and premenopausal women and determine the effect of parity in postmenopausal women.
Materials and Methods
Study design
The study is a case and control study of post-menopausal volunteers attending clinics at Saint Philomena Catholic Hospital in Benin City Nigeria.
Ethical consideration
Ethical approval was sought for and obtained from the Saint Philomena Catholic Hospital Health Ethics Review Committee and from the management of the hospital. Similarly, informed consent was obtained after provision of adequate, clear and complete information about what the study entails to the participant and they were informed that involvement in the study is voluntary and before enrolment into the study, informed consent will be signed by all participants. The study was conducted in compliance with the Declaration on the Right of the subject/participant [17]. Confidentiality of data was ensured by not including name of the participants or any information in connection with them.
Site of the study
The study was conducted in the obstetrics and gynecology department of Saint Philomena Hospital, Benin City-Nigeria. The Saint Catholic Philomena Hospital is a catholic hospital located at 23 Dawson Road, in Benin City, Edo State. The hospital was established in February 1941, as a biblical mustard seed by the catholic Bishop of Benin City, Bishop Patrick Joseph Kelly. Over the years, the hospital has grown to provide medical services in gynecology, obstetrics, internal medicine, surgery, dentistry, ophthalmology, dermatology and physiotherapy.
Study population
The study is targeted at all post-menopausal volunteers attending clinic at the department of obstetrics and gynecology of the Saint Catholic Philomena Hospital. In this study, the occurrence of an event (post-menopause women) made us to search for exposure to a determined factor (parity). In the resent study, we tried to match women in each of the determined factor (parity) with the control by selecting 40 subjects each in the determined factor and these included premenopausal women, nulliparous postmenopausal women, and postmenopausal women with parity ranging from one to six and above.
Inclusion criteria
The criteria for participating in the study were all medically diagnosed post-menopausal women within the ages of 49 and 69 who are apparently healthy and currently not undergoing any treatments on chronic illnesses.
Exclusion criteria
The criteria for excluding a participant who may want to participant in the study include all those with history of pathologically influenced menopause, assisted reproductive technique, surgical induced menopause, chemotherapy, those on hormone replacement therapy, bad obstetric history and those chronically ill as well as patients who have been on medications for over four weeks. In addition, those shown to present other chronic illness and are currently on other drugs were excluded from the study. Subjects less than 49 years and above 70 years were excluded from the study. All patients who fail to give consent to be included in the study were also be excluded from the study.
Sampling procedures
In a bid to achieve the objectives, post-menopausal women currently attending clinic in the Department of obstetrics and gynecology, were invited to take part in the study by visiting case notes and inviting them for data collection. In this regard, the convenient sampling method was employed for recruiting subjects who meet the study criteria into the study after clinically confirming menopause and gave consent. The disadvantage of this sampling method is that only women who honored the invite will be included in the study and as such, the results may not give a representation of the population. The inclusion of women into each group was terminated when date of 40 women have been gotten. This also may affect the results of this study.
Sample collection
Data and sample were obtained from those who gave consent to be included in the study were required to complete a questionnaire. A structured questionnaire containing their biodata, gynaecology history, past medical and obstetric history was administered and at the end blood sample was obtained following standard laboratory procedures.
Sample analysis
All materials used for this study were standard. Measurement of anthropometric parameters: Height was measured in meters using a standard standiometer (Avery Barked, UK). Weights were measured in kilograms using weighing scale (Avery Berked, UK). The body mass index was calculated using the formula; Weight in Kilogram/Height in meter 2(Wt/Ht2).
Estimation of serum calcium and phosphate: Serum calcium was estimated by using spectrophotometer methods following the procedures previously outline by Tietz [18,19]. Inorganic phosphorus was estimated following the methods by Daly and Ertingshausen [20] using the spectrophotometer.
Data analysis
The data obtained were analysis using the Statistical Package for Social Sciences (SPSS) version 20. The data were subjected to descriptive statistic (frequency, percentage and mean) and inferential statistics (“t-test”) and statistical difference was determined at a confidence interval of 95% and p<0.05 was considered significant.
Results
Table 1 shows the biological profile of the women that participated in the study. There was a significant different in the mean age (31.73 ± 11.45 years vs. 57.06 ± 5.57 years), weight (60.49 ± 17.17 Kg vs. 67.30 ± 15.68 Kg) and body mass index (25.42 ± 4.16 Kg/M2 vs. 27.60 ± 4.32 Kg/M2) between the premenopausal women and postmenopausal women but there was no significant different in their height (1.51 ± 0.37M vs. 1.56 ± 0.11M). Table 2 compared serum calcium and phosphate in premenopausal and postmenopausal women. There was a significant decrease (p<0.05) in serum calcium (11.07 ± 1.53 mg/ dl vs. 8.20 ± 0.41 mg/dl) but a significant increase (p<0.05) in serum phosphate (2.39 ± 0.45 mg/dl vs. 3.71 ± 0.71 mg/dl) in postmenopausal women compared to premenopausal women. In fact, the decrease in serum calcium and increase in serum phosphate in postmenopausal women were by 25.93% and 55.23% respectively. Table 3 presents the effect of parity on serum calcium and phosphate in postmenopausal women.
| Groups | N | Age (years) | Height (M) | Weight (Kg) | BMI (Kg/m2) |
|---|---|---|---|---|---|
| Premenopausal | 40 | 31.73 ± 11.45 | 1.51 ± 0.37 | 60.49 ± 17.17 | 25.42 ± 4.16 |
| Postmenopausal | 280 | 57.06 ± 5.57* | 1.56 ± 0.11 | 67.30 ± 15.68* | 27.60 ± 4.32* |
N=320; values are mean ± standard deviation; * indicates significant different at p<0.05 compared to Pre-M=pre-menopausal women (n=40); Post-M=post-menopausal women (n=280).
Table 1: Biological profile of the women participating in the study.
| Groups | Ca2+(mg/dl) | PO4(mg/dl) |
|---|---|---|
| Pre-M | 11.07 ± 1.53 | 2.39 ± 0.45 |
| Post-M | 8.20 ± 0.41* | 3.71 ± 0.71* |
| % declined/increase | 25.93 | 55.23 |
N=320; values are mean ± standard deviation; * indicates significant different at p<0.05 compared to Pre-M=pre-menopausal women (n=40); Post-M=post-menopausal women (n=280).
Table 2: Comparative evaluation of serum calcium and phosphate between pre-menopausal and post-menopausal women.
| Groups | Serum calcium (mg/dl) | Serum phosphate (mg/dl) |
|---|---|---|
| Nulliparous postmenopausal | 8.11 ± 0.39 | 2.66 ± 0.09 |
| Parous postmenopausal | 8.21 ± 0.32 | 3.88 ± 0.52* |
N=280; values are mean ± standard deviation; * significant different at p<0.05.
Table 3: The effect of parity on serum calcium and phosphate in post-menopausal women.
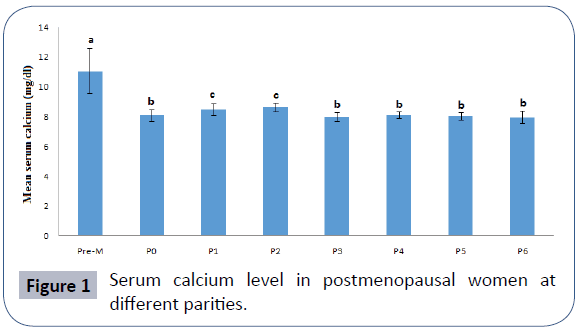
It was observed that serum calcium was non-significantly higher (8.11 ± 0.39 mg/dl vs. 8.21 ± 0.32; p>0.05) but serum phosphate significantly higher (2.66 ± 0.09 mg/dl vs. 3.88 ± 0.52 mg/dl; p<0.05) in parous postmenopausal women compared to nulliparous postmenopausal women. Figure 1 compares serum calcium level (mg/dl) in the menopausal women at different parity groups compared with premenopausal women. Comparatively, serum calcium activity in postmenopausal women were significantly lower (p<0.05) compared to premenopausal women. Compared to nulliparous menopausal women (8.11 ± 0.39 mg/dl), menopausal women in their 1st (8.49 ± 0.39 mg/ dl) and 2nd (8.64 ± 0.31 mg/dl) parities have significantly higher mean serum calcium level while those in 6+ parity group (7.96 ± 0.42 mg/dl) has significantly lower mean serum calcium level.
Figure 1: Serum calcium level in postmenopausal women at different parities.
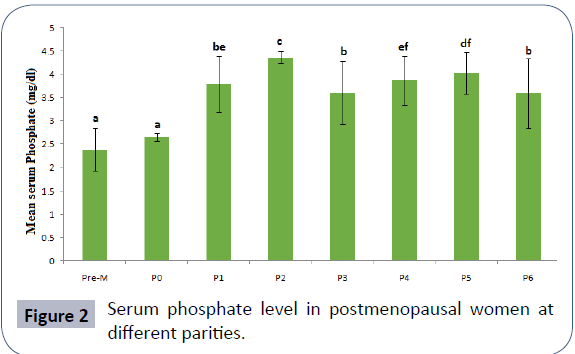
N=320; values are mean ± standard deviation; means with different superscripts are significantly different at p<0.05, Pre- M=premenopausal women, P0=Nulliparous postmenopausal women, P1-P6= Postmenopausal women with parity ranging from one to six plus. Figure 2 compares serum phosphate level in menopausal women based on parity compared with premenopausal women. Comparatively, serum phosphate activity in postmenopausal women were significantly higher (p<0.05) compared to premenopausal women except in the nulliparous postmenopausal women where the different was not significant (p>0.05). Irrespective of the number of parity, mean serum phosphate level was significantly lower among nulliparous menopausal women (2.66 ± 0.09 mg/dl). Serum phosphate level was highest among post-menopausal women with 2 parities (3.79 ± 0.62 mg/dl) and this was followed by those with 5 parities (4.03 ± 0.45 mg/dl) and then those with 4 parities (3.88 ± 0.53 mg/dl). N=320; values are mean ± standard deviation; means with different superscripts are significantly different at p<0.05, Pre-M=premenopausal women, P0=Nulliparous postmenopausal women, P1-P6=Postmenopausal women with parity ranging from one to six plus
Figure 2: Serum phosphate level in postmenopausal women at different parities.
Discussion
The present study compared serum calcium and phosphate in premenopausal and postmenopausal women and determined the effect of parity on these parameters in postmenopausal women. The findings of the study showed that postmenopausal women have a 25.93% deficit in serum calcium but a 55.23% surfeit of serum phosphate compared with premenopausal women. Specifically, this study found that serum calcium decreases in postmenopausal women (8.20 ± 0.41 mg/dl) when compared to premenopausal women (11.07 ± 1.53 mg/dl) with a statistically significant. This finding is consistent with the study [21] who carried out a hospital based preliminary study in postmenopausal women. In agreement with our results, a study had also reported a significant decrease (p<0.00001) in serum calcium activity in post menopausal women (8.80+0.89 mg/dl) compared to premenopausal women (10.07+0.66 mg/dl) [1]. This observation is in line considering that lack of estrogen causes bone resorption in postmenopausal women preventing the absorption and utilization of bone calcium and hence the reduced serum calcium level in these women. On serum phosphate, we found that serum level increase significantly in postmenopausal women (3.71 ± 0.71 mg/dl) compared to premenopausal women (2.39 ± 0.45 mg/dl) and this is consistent with the findings [1] who found that phosphorus levels significantly increased (p<0.001) in menopausal women (4.07+1.09 mgs/dl) compared to controls (3.72+0.56 mgs/dl). The observed effects of menopause on bone mineralization may be due to the fact [22] that declining ovarian function in menopause is accompanied by reduction in bone mass and altered calcium metabolism. In fact, estrogen deficiency has been reported to induce calcium loss due to decreased intestinal calcium absorption and decreased renal calcium conservation [23,24]. Thus, the characteristic feature of menopause indicated via reduction in skeletal mass caused by an imbalance between bone formation and bone resorption due to loss of ovarian function.
On the effect of parity, we observed that parity has a nonsignificantly increase on serum calcium but a significant increase on serum phosphate compared to the nulliparous postmenopausal women. Specifically, we observed that postmenopausal women in their 1st and 2nd parities have significantly higher serum calcium level than nulliparous postmenopausal while postmenopausal women in their 3rd through 6th parities presented non-significantly difference in serum calcium compared with the nulliparous postmenopausal women. On the other hand, serum phosphate was highest in postmenopausal women with two parities and was significantly higher compare with the nulliparous postmenopausal women. In fact, we observed that serum phosphate was lower among postmenopausal women with 3 to 6 parities compared to postmenopausal women with one or two parities. These findings suggest that pregnancy may influence serum calcium and phosphate levels in postmenopausal women and by implication influence bone mineralization. Several changes occur during pregnancy and lactation that can affect bone mass, including changes in reproductive hormones and in hormones that affect calcium metabolism. Since fetal and infant bone growth during pregnancy and lactation depends on calcium transfer from the mother, the possibility that pregnancy and lactation affect risk for bone mineral loss later in life has been investigated [15].
In this regard, epidemiologic studies indicated that neither extended lactation nor multiple pregnancies are associated with subsequent osteoporosis, whether measured by BMD levels or by assessment of fracture risk [25] and that having more children does not appear to increase fracture risk [26]. On the other hand, some studies reported the risk of hip fracture to decrease by 5-10 percent with each additional child, and there is no apparent association between the duration of lactation and fracture risk [27]. In the same line some researchers’ belief that, pregnancy and lactation in healthy adult women do not appear to cause lasting harm to the skeleton as women with more than 10 pregnancies and extended lactation had BMD levels similar to women who have not been pregnant. However, in the present study, we found that having either one or two children may positively influence bone mineral in postmenopausal life while having more than two children may have negative effect on bone mineralization indicated via serum calcium. In compares with the findings of this study, a review of 19 studies [15] found, six studies (with a combined total of 17,077 subjects) to show a positive effect of parity on BMD in postmenopausal women while eight studies supported a negative effect of parity on BMD in postmenopausal women (with a combined total of 7,410 subjects) and five studies (with a combined total of 2,947 women) did not find any effect.
Conclusion
Base on the findings of this study, we re-established that bone minerals are negatively affected by menopause and that parity might have effect. Our findings showed that either one or two children or pregnancy might have positive influence on body minerals during the postmenopausal life. However, this effect may have some confounding factors that are not considered in this study.
Acknowledgment
The authors thank the study participants and the assistance rendered by hospital staff and research assistants.
References
- Prabha YS, Ashalata K, Vijaya Babu PVSS, Kumari PK, Nagamani M (2015) A Study of bone markers (Serum calcium, Serum phosphorus and Serum alkaline phosphatase) in post-menopausal women in east Godavari District, Andhra Pradesh, India. IOSR Journal of Dental and Medical Sciences 14: 1-3.
- Mishra S, Manju M, Toora BD, Mohan S, Venkatesh BP (2015) Comparison of bone mineral density and serum minerals in pre and post-menopausal women. Int J Clin Trials 2: 85-90.
- Deepthi SK, Amar Raghu Narayan G, Naidu JN (2012) Study of biochemical bone turnover markers in postmenopausal women leading to osteoporosis. Int J Appl Biol Pharmaceut Technol 3: 301-305.
- Riggs BL, Khosla S, Melton LJ (2002) Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev 23: 279-302.
- Svedbom A, Hernlund E, Ivergård M, Compston J, Cooper C, et al.(2013) EU review panel of IOF osteoporosis in the European Union: A compendium of country-specific reports. Arch Osteoporos 8: 137.
- Liu YJ, Zhang L, Papasian CJ, Deng HW (2014) Genome-wide association studies for osteoporosis: A 2013 update. J Bone Metab 21: 99-116.
- Nachtigall MJ, Nazem TG, Nachtigall RH, Goldstein SR (2013) Osteoporosis risk factors and early life-style modifications to decrease disease burden in women. Clin Obstet Gynecol 56: 650-653.
- Hosie CJ, Hart DM, Smith DA (1989) Differential effect of long-term oestrogen therapy on trabecular and cortical bone. Maturitas 11: 137-145.
- Lenora J, Lekamwasam S, Karlsson MK (2009) Effects of multiparity and prolonged breast-feeding on maternal bone mineral density: A community-based cross-sectional study. BMC Womens Health 1: 19.
- Hillier TA, Rizzo JH, Pedula KL, Stone KL, Cauley JA, et al.(2003) Nulliparity and fracture risk in older women: The study of osteoporotic fractures. J Bone Miner. Res 18: 893-899.
- Cure-Cure C, Cure-Ramírez P, Terán López-Jaramillo P (2002) Bone-mass peak in multiparity and reduced risk of bone-fractures in menopause. Int J Gynaecol Obstet 76: 285-291.
- Ozdemir F, Demirbag D, Rodoplu M (2005) Reproductive factors affecting the bone mineral density in postmenopausal women. Tohoku J Exp Med 205: 277-285.
- Gur A, Nas K, Cevik R, Sarac AJ, Ataoglu S, et al. (2003) Influence of number of pregnancies on bone mineral density in postmenopausal women of different age groups. J Bone Miner Metab 21: 234-241.
- Reed SD, Scholes D, La Croix AZ, Ichikawa LE, Barlow WE, et al. (2003) Longitudinal changes in bone density in relation to oral contraceptive use. Contraception 68: 177-182.
- Bayray A, Enquselassie F (2013) The effect of parity on bone mineral density in postmenopausal women: A Systematic review. J Osteopor Phys Act 1: 104.
- Kalkwarf HJ, Specker BL (2002) Bone mineral changes during pregnancy and lactation. Endocrine 17: 49-53.
- World Medical Association Declaration of Helsinki (2000) Ethical principles for medical research involving human subjects.
- Tietz NW (1996) Fundamentals of clinical chemistry, 4 (Ed) WB Saunders, Philadelphia.
- Daly JA, Ertingshansen G (1972) Simply serum phosphorous analysis plifiedSerum phosphorus analyses by continuous-flow ultraviolet spectrophotometry. Clinical Chemistry pp: 18-263.
- Indumati V, Vidya SP, Rama J (2007) Hospital based preliminary study on osteoporosis in postmenopausal women. Indian Journal of Clinical Biochemistry 22: 96-100.
- Garton M, Martin J, New S, Lee S, Loveridge N, et al. (1996) Bone mass and metabolism in women aged 45-55. Clin Endocrin 44: 563-573.
- Uebelhart D, Schlemmer A, Johansen JS, Gineyts E, Christiansen C, et al. (1991) Effect of menopause and hormone replacement therapy on the urinary excretion of pyridinium cross-links. J Clin/Endocrinal Metab 72: 367-373.
- Gennari C, Agnusdei D, Nardi P, Citvitelli R (1990) Estrogen preserves a normal intestinal responsiveness to 1.25-dihydroxy vitamin D3 in oophorectomized women. J Clin/ Endocrinal Metab 71: 1288-1293.
- Karlsson C, Obrant KJ, Karlsson M (2001) Pregnancy and lactation confer reversible bone loss in humans. Osteoporos Int 12: 828-834.
- Cumming RG, Klineberg RJ (1993) Breastfeeding and other reproductive factors and the risk of hip fractures in elderly women. Int J Epidemiol 22: 684-691.
- Michaelsson K, Baron JA, Farahmand BY, Ljunghall S (2001) Influence of parity and lactation on hip fracture risk. Am J Epidemiol 153: 1166-1172.
- Henderson PH, Sowers M, Kutzko KE, Jannausch ML (2000) Bone mineral density in grand multiparous women with extended lactation. Am J Obstet Gynecol 182: 1371-1377.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences