Acute Kidney Injury, Hypercalcemia and a Lung Mass
1Department of Medicine, Western Sydney University, Australia
2Department of Radiology, Western Sydney University, Australia
3Department of Nephrology, School of Medicine, Western Sydney University, Australia
- *Corresponding Author:
- Surjit Tarafdar
Department of Medicine, Western Sydney University, Australia
Tel: +61 424127991
E-mail: Surjit.Tarafdar@health.nsw.gov.au
Received date: December 12, 2018; Accepted date: January 9, 2019; Published date: January 15, 2019
Citation: Tarafdar S, Mikaheal Y, Alqutawneh B, Kairaitis L (2018) Acute Kidney Injury, Hypercalcemia, and a Lung Mass. Jour Ren Med Vol.3 No. 1:1.
Copyright: © 2019 Tarafdar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Plasma cell dyscrasias are characterized by neoplastic proliferation of a single clone of plasma cells typically producing a monoclonal immunoglobulin. Plasma cell neoplasms can present as a single lesion (solitary plasmacytoma) or more commonly as multiple lesions (multiple myeloma). Plasmacytomas can be present at the initial diagnosis of multiple myeloma or develop later during the course of the disease.
When plasmacytoma is associated with 10 percent or more clonal plasma cells in the bone marrow, the diagnosis is considered to be multiple myeloma rather than solitary plasmacytoma. While solitary plasmacytomas are treated with radiotherapy, multiple myeloma is treated with chemotherapy.
Introduction
A 64-year-old male with a background of renal biopsy-proven chronic kidney disease stage III due to diabetic nephropathy presented with a 10-week history of increasing lethargy, poor appetite, and 30 kg unintentional weight loss. The patient was an ex-smoker with a 30-pack year smoking history.
Examination revealed normal vital signs with no fever, decreased air entry in the left lung apex and normal cardiovascular and abdominal examination.
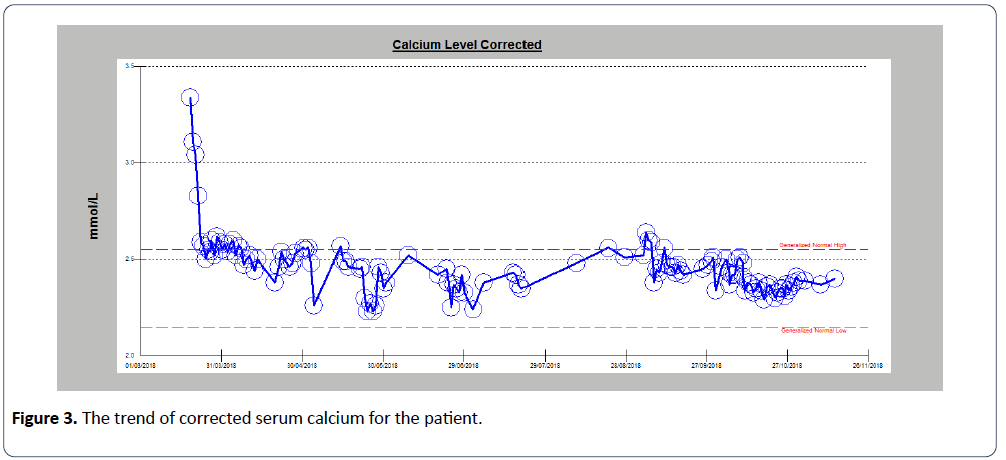
Blood tests demonstrated acute kidney injury with a serum creatinine of 702 μmol/l (reference range: 60 μmol/l-110 μmol/l), an estimated glomerular filtration rate of 6 mL/min/ 1.73 m2, hemoglobin of 77 g/L (reference range: 130-180 g/L) and corrected calcium of 3.34 mmol/L (reference range: 2.15 mmol/L-2.55 mmol/L). The serum parathyroid hormone level was suppressed to 1.3 pmol/L (reference range: 1.6 pmol/L to 7.5 pmol/L) ruling out hyperparathyroidism as the cause of hypercalcemia. Serum Parathyroid Hormone-related Protein (PTHrP) which is characteristically raised in hypercalcemia associated with solid organ malignancy was reported normal at <2.0 pmol/L. The platelet counts, white blood cell count and mean corpuscular volume were all in the normal range. Liver function tests were unremarkable.
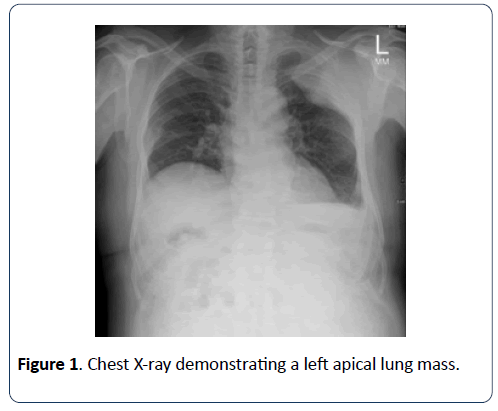
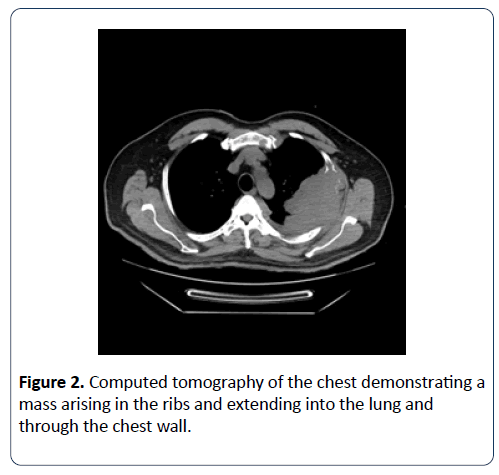
Chest X-ray revealed a large left upper lobe mass which was followed by computed tomography (CT) of his chest (Figures 1 and 2).
The patient denied any exposure or history of tuberculosis. Given the smoking history, significant weight loss, hypercalcemia and radiological finding, the initial presumptive diagnosis was lung cancer. The on-call hematologist reported marked rouleaux formation and circulating plasmacytoid lymphocytes on the blood film. Further blood tests demonstrated an elevated total protein level of 122 g/L (reference range, 46-70 g/L) with a predominant elevation in the globulin fraction. Though the chest X-ray was reported as a left upper lung mass with rib destruction suggesting lung cancer, the CT scan reported the lesion as originating from the ribs and unlikely to be lung cancer.
Subsequently, a bone marrow biopsy was performed that confirmed the diagnosis.
Diagnosis
Multiple myeloma: The combination of the radiological finding of a mass originating in the ribs and eroding into the lung, raised serum globulin fraction and marked rouleaux formation with circulating plasmacytoid lymphocyte cells seen on the blood film raised the possibility of a plasmacytoma originating in the ribs on a background of multiple myeloma. Subsequently, serum protein electrophoresis revealed a raised IgA kappa paraprotein at 55 g/L (ref range: 0.8 to 4.40 g/L).
Testing for Serum Free Light Chains (SFLC) revealed a markedly elevated level of kappa light chain to 5597.0 mg/L (ref range: 3.30 mg/l to 19.40 mg/l) with a grossly elevated kappa to lambda ratio of 553 (involved/uninvolved SFLC ratio of 100 or more diagnostic for myeloma). Bone marrow biopsy demonstrated greater than 45% clonal plasma cells, supporting the diagnosis of multiple myeloma.
The patient was commenced on high dose dexamethasone followed by chemotherapy (Cyclophosphamide-Bortezomib- Dexamethasone) in consultation with the hematology services. The hypercalcemia responded well to intravenous therapy with normal saline and did not need the introduction of any other agent (Figure 3).
Solitary plasmacytomas occur in bone (plasmacytoma of bone) or less commonly in soft tissues (extramedullary plasmacytoma). 7%-18% of patients with multiple myeloma have a plasmacytoma present at the time of initial diagnosis while another 6%-20% develop a plasmacytoma during the course of their disease [1].
Solitary Plasmacytoma of Bone (SPB) is a localized tumor in the bone comprised of a single clone of plasma cells in the absence of other features of multiple myeloma (i.e. anemia, hypercalcemia, renal insufficiency, or multiple lytic bone lesions). The bones most commonly involved are those with active hematopoiesis. The bone sites involved in decreasing order of frequency are vertebrae, pelvis, ribs, upper extremities, face, skull, femur, and sternum [2]. The primary treatment for patients with SPB in the absence of multiple myeloma is localized radiation therapy.
The less common Solitary Extramedullary Plasmacytomas (SEP) are non-osseous plasma cell tumors that arise outside of the bone marrow. Approximately 80 percent involve the upper respiratory tract (i.e. oronasopharynx and paranasal sinuses), producing epistaxis, nasal discharge or nasal obstruction while other sites of involvement include lung, liver, gastrointestinal tract, central nervous system, testes, and skin [3,4]. In the absence of features of myeloma, treatment consists of radiation therapy.
If patients with plasmacytomas have 10 percent or more clonal plasma cells in the bone marrow, they are considered to have multiple myeloma rather than solitary plasmacytoma and treated with anti-myeloma chemotherapy rather than radiation therapy [5].
Lessons from this case
1. A lung mass in a patient with a strong smoking history and hypercalcemia would be assumed to be lung cancer. However, the radiological findings of the mass originating from the bone rather than lung, paraprotein elevation, and bone marrow findings led to the diagnosis of multiple myeloma
2. When plasmacytoma is associated with 10 percent or more clonal plasma cells in the bone marrow, the diagnosis is considered to be multiple myeloma rather than solitary plasmacytoma
3. It is vital to differentiate between solitary plasmacytomas and multiple myeloma as the treatment options differ, being radiotherapy in the former and chemotherapy for the later
References
- Bladé J, de Larrea CF, Rosiñol L (2012) Extramedullary involvement in Multiple Myeloma. Haematologica 97: 1618–1619.
- Ozsahin M, Tsang RW, Poortmans P, Belkacémi Y, Bolla M, et al. (2006) Outcomes and patterns of failure in solitary plasmacytoma: a multicenter Rare Cancer Network study of 258 patients. Int J Radiat Oncol Biol Phys 64: 210.
- Prasad R, Verma SK, Sodhi R ( 2011) Multiple myeloma with lung plasmacytoma. Lung India 28: 136–138.
- Galieni P, Cavo M, Avvisati G, Pulsoni A, Falbo R, et al. (1995) Solitary plasmacytoma of bone and extramedullary plasmacytoma: two different entities? Ann Oncol.6: 687-691.
- Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, et al.(2014) International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol15: e538-548.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences