ISSN : 2393-8862
American Journal of Pharmacology and Pharmacotherapeutics
A Case Report on Hydroxychloroquine Drug Induced Maculopappular Rashes: Immunosuppressants and Corticosteroid Therapy
Sunil Kumar S*
Department of Pharmacy, Santhiram College of Pharmacy, Andhra Pradesh, India
- *Corresponding Author:
- Sunil Kumar S
Department of Pharmacy, Santhiram College of Pharmacy, Andhra Pradesh, India
Tel: +6302926232
E-mail: sunilkumarteluguu@gmail.com
Received Date: July 06, 2019; Accepted Date: August 20, 2019; Published Date: August 26, 2019
Citation: Kumar SS (2019) A Case Report on Hydroxychloroquine Drug Induced Maculopappular Rashes: Immunosuppressants and Corticosteroid Therapy. Am J Pharmacol Pharmacother Vol.6 No.1:2.
Abstract
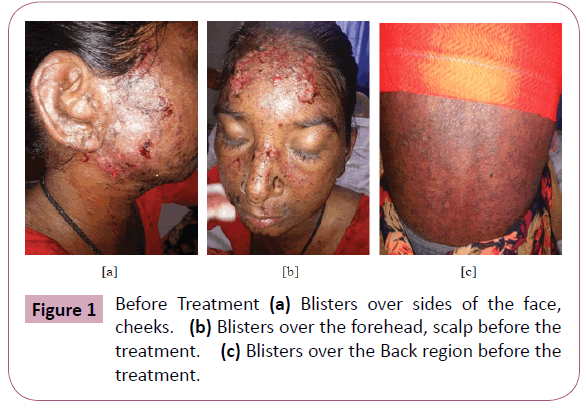
Maculopappular rashes are the cutaneous eruptions that are associated with erosions and bleeding of cutaneous lesions over the body. In this case study a 45-year-old female patient has developed Maculopappular rashes over the body. It is a clinical reaction due to the medication like Hydroxychloroquine which have been used by the patient for the joint pains. Simultaneously development of blisters over the forehead, scalp, upper and lower limbs which eventually get ruptured and forms erosions. This episode was mainly due to the repeat drug intake of Hydroxychloroquine for the joint pains as a daily regimen, this Hydroxychloroquine has a known cause of pustules excisional biopsy of the ruptured erosions was performed and confirmed as Maculopappular rashes. The patient was treated with Immunosuppressants, Systemic and topical corticosteroids for more than 1 month to control and completely cure the rashes.
Keywords
Blisters; Maculopappular; Pustulosis; Erythematous; Erosions
Introduction
Maculopappular rashes are the cutaneous eruptions that are associated with erosions and bleeding of cutaneous lesions over the body. In this case study a 45-year-old female patient has developed Maculopappular rashes over the body. It is a clinical reaction due to the medication like Hydroxychloroquine which have been used by the patient for the joint pains. Simultaneously development of blisters over the forehead, scalp, upper and lower limbs which eventually get ruptured and forms erosions. This episode was mainly due to the repeat drug intake of Hydroxychloroquine for the joint pains as a daily regimen, this Hydroxychloroquine has a known cause of pustules excisional biopsy of the ruptured erosions was performed and confirmed as Maculopappular rashes. The patient was treated with Immunosuppressants, Systemic and topical corticosteroids for more than 1 month to control and completely cure the rashes.
Muculopappular rashes are uncommon, cutaneous eruptions which is characterized by erosions and bleeding of lesions over the body. The drugs which are commonly implicated in causery pustulosis are antibiotics like macrolides cephalosporins and Aminopencillins [1]. Hydroxychloroquine shows effective therapeutics action on inflammatory arthritis and erythematous lupus [2]. In this case Hydroxychloroquines is reported to cause pustulosis, shortly after the discontinuation of the drug [3-7] having the close characteristics of maculopustulosis for 15 days due to other medications. Here mainly due to the discontinuation of the offending agent shows complete resolution for 15 days. The lesions get ruptured to form crusts on the body surface due to ulcerations which are very painful. We are reporting that it is a Hydroxychloroquine drug induced Maculopappular rashes and received systemic and topical Corticosteroids therapy successfully and discharged for 21 days.
Case Report
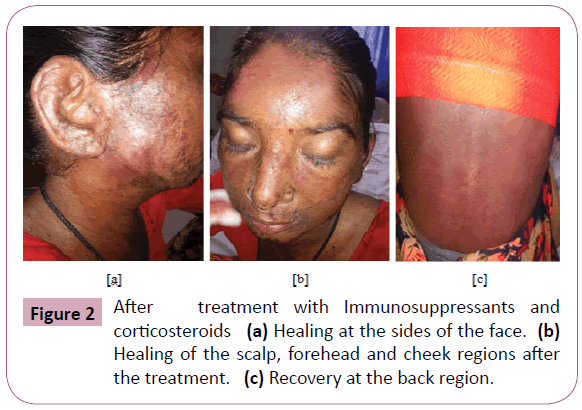
A 45-year-old female patient was apparently normal 5 months back presented with chief complaints high grade fever with chills and joint pains for which she consulted doctor and got treated, where the fever was subsided but there was intermittent episodes of fever and consulted same physician and repeated the treatment for 2 months. As the problem did not subside they consulted another private hospital and were prescribed Hydroxycloroquine for about 2 weeks. She developed vomitings and blisters over sides of the face, cheeks which ruptured and forms erosions [3-7]. So they again went to government hospital for those complaints and they have given fluid replacement therapy and stayed there for one day. There was simultaneous development of blisters over the forehead, scalp, rashes, upper and lower limbs and redness over the conjunctiva since 4-5 days with itching. This multiple erythematous papules over the body varying 0.5 × 0.5 cm to 2 × 3 cm size and oozing. Patient went to private medical practitioner got medicated and was referred to the tertiary care teaching hospital for further treatment. The patient was treated with Immunosuppressants, systemic and topical corticosteroids; for certain pain reliefs providing local anesthetics like benzocaine. Also providing continuous vital supplements and Antibiotics (Figures 1 and 2).
Discussion
Maculopappular rashes are the cutaneous eruptions which are composed of subcorneal and intraepidermal pustules. The appearance of the reaction is similar to that of pustular psoriasis with pustules, overlying flaking and scaling the skin. In this case the multiple erythematous papules are observed over the sides of the face, cheeks, forehead, scalp and upper and lower limbs.
She is also having scattered erythematous macules and papules over the thighs, legs and plantar surface of the feet. A biopsy taken from the forehead demonstrated that subcorneal pustular dermatosis on examination there was a multiple discrete erythematous plaques on face and extended to the lower extremities. Acute and repeated ulceration can add to systemic upset and possibility of compromised life [8-10]. The diagnosis of maculopappular rashes is based on the history of clinical presentation and histopathologic features. Where the laboratory investigations are non-specific. To consider differential diagnosis include pustular psoriasis, subcorneal pustulosis and drug reaction with eosinophiles and systemic symptoms clinically maculopappular rashes are similar to pustular psoriasis having a history of shorter duration of pustules, fever and administration of new medication. Multiple erythematous papules get ruptured and form a crust these are treated with immunosuppressants, systemic, topical corticosteroids Antibiotics and some vital supplements these rashes may leads to benign self-limiting course and get erupted as superficial desquamation. Systemic corticosteroids like Prednisolone was given and this may often treated for maculopustulosis with variable results [5]. Immunosuppressants like cyclosporines has a prompt recovery [3] topical corticosteroids like triamcinolone is used to relieve the symptoms such as pain, swelling and various skin and allergic disorders. For immediate pain relief some local Anaesthetics like Benzocaine was provided due to the severity of Eruptions Antibiotics like cefixime was given to prevent bacterial infections. Continuous vital supplements were provided due to excessive fluid discharge from the body over the rashes. At a follow-up of 3 weeks there were no recurrence of any lesions on the skin with this therapy and the patient was currently under the review.
Conclusion
In these exploratory clinical studies it was proved that safety and efficacy of the drugs used in this patient for the treatment of Hydrochloroquine induced maculopappular rashes. Corticosteroids and immunosuppressants are most commonly used drugs in the management of maculopappular rashes. Which are drug induced cutaneous reactions. We are reporting that lesions on the body get treated by this therapy where the patient conditions get normalized. The results need to be further confirmed in a larger randomized controlled clinical trials which is an on-going process in our tertiary care teaching hospital.
Acknowledgement
The authors want to thank the Dean, Teaching and Non-teaching staff of the Santhiram Medical college and General hospital for the help and support of our study. We also thank the Santhiram college of Pharmacy to provide and facilitate the hospital speciality.
References
- Sanofi-Aventis (2018) Product monograph: Plaquenil.
- Centers for Disease Control and Prevention (CDC) (2018) Malaria information and prophylaxis, by country.
- Wallace DJ (1996) The history of antimalarials. Lupus 5: S2-S3.
- Shee JC (1953) Lupus erythematosus treated with chloroquine. Lancet 265: 201-202.
- Kuznik A, Bencina M, Svajger U, Jeras M, Rozman B, et al. (2011) Mechanism of endosomal TLR inhibition by antimalarial drugs and imidazoquinolines. J Immunol 186: 4794-804.
- Willis R, Seif AM, McGwin G Jr., Martinez-Martinez LA, González EB, et al. (2012) Effect of hydroxychloroquine treatment on pro-infl ammatory cytokines and disease activity in SLE patients: Data from LUMINA, a multiethnic US cohort. Lupus 21: 830-835.
- Fox R (1996) Anti-malarial drugs: Possible mechanisms of action in autoimmune disease and prospects for drug development. Lupus 5: S4-S10.
- Williams PM, Corklin RJ (2005) Erythema Multiforme: A review and contrast from Stevens-Johnson syndrome/toxic epidermal necrolysis Dent Clin N Am 49: 67-76.
- Kohli PS, Kaur J (2011) Erythema Multiforme-oral variant: Case report and review of literature. Indian J Otolaryngol Head Neck Surg 63: 9-12.
- Bharati P, Sushmini H, Shobha N, Rakesh S (2013) Oral blistering. A report of two cases of Erythema Multiforme & literature review. J Clin Diagn Res 7: 2080-2083.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences