Page 45
May 24-25, 2018
London, UK
Vascular Surgery 2018
3
rd
Edition of World Congress & Exhibition on
Vascular Surgery
Journal of Vascular and Endovascular Therapy
ISSN: 2573-4482
Introduction:
Duplex scanning is currently the best method to
detect stenotic lesions that threaten bypass graft patency. The
correction of these lesions may improve long term patency of
grafts and limb salvage rates. The aimof this study is to investigate
the effects of duplex surveillance post femoro-popliteal bypass
graft for chronic limb threatening ischemia (CLTI) in terms of graft
patency and limb salvage.
Methodology:
A retrospective analysis of 59 patients who had
underwent femoro-popliteal bypass graft for CLTI between Jan
2009 and April 2014. Data was collected from the electronic
computer record and analyzed using SPSS v24.
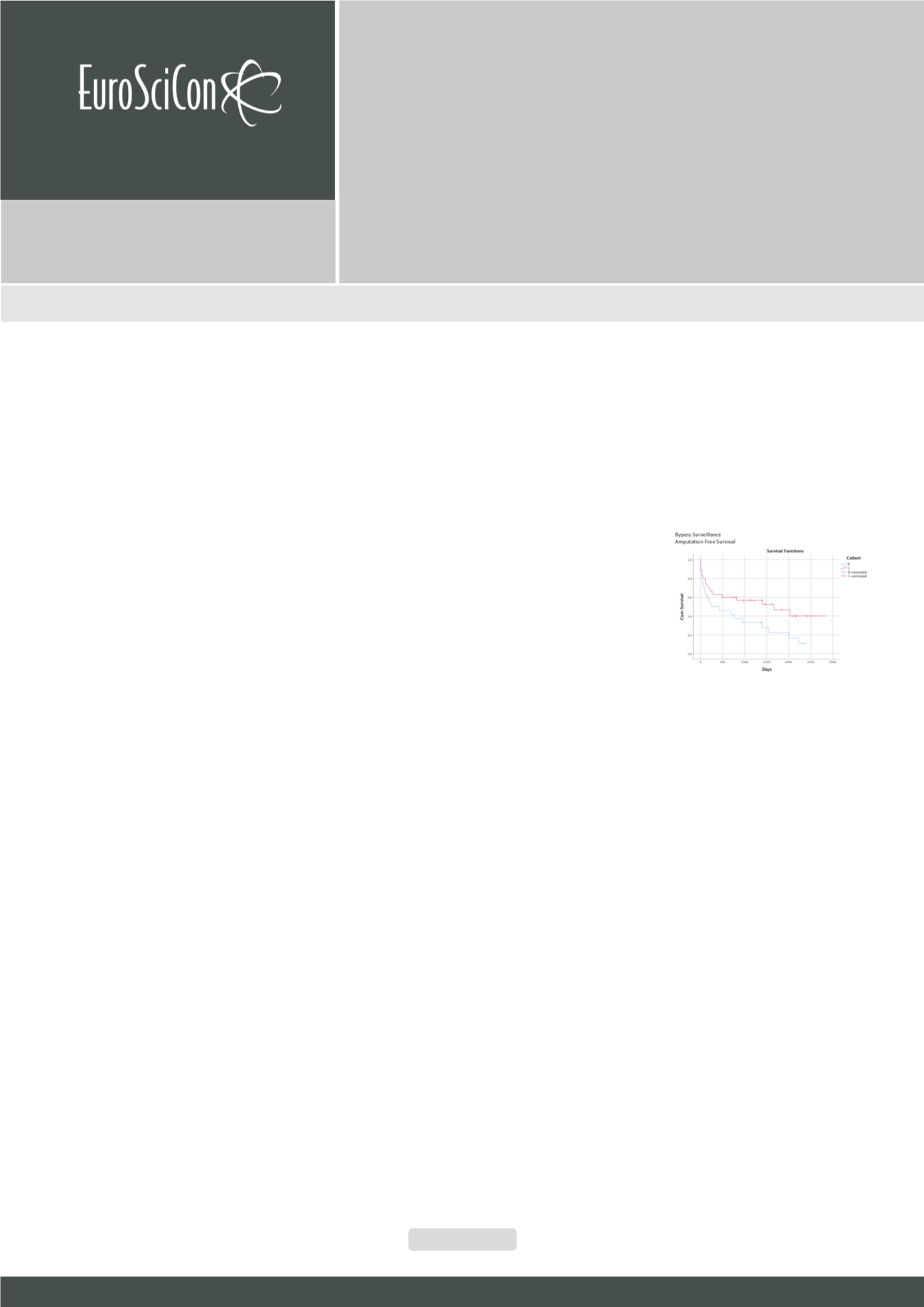
Results:
Of 59 patients; 49 (83.1%) had autologous vein graft, 8
(13.6%) prosthetic vein grafts and 2 (3.4%) composite graft. Mean
follow up was 13.6 (0-64) months. Mean age was 77 (58-96) years.
Duplex scan surveillance was performed in 35 (71.4%) patients
at 3, 6, 9, 18 and 24 months post operatively; 27 in autologous
vein, 7 in prosthetic graft and 1 in composite. Positive findings of
occluded graft were noted in 10 duplex scans; all blocked grafts
were autologous vein grafts. Out of the 17 patent vein grafts,
stenosis was noted in 9 veins requiring angioplasty. Two patients
needed amputation after angioplasty. Primary patency at 1 and 2
yrs. for duplex surveillance group was 71.4% and no surveillance
group was 54.2%. Within two years 21 patients needed major
amputation. Total amputation rate was 35.5%. Ten amputations in
patient who were on surveillance were 28.5% and eleven who had
no surveillance were 45.8%. At 7 years amputation free survival
(AFS) was 48.6% vs. 16.7% in no surveillance group (HR 0.52 95%
CI 0.28-0.99 p=0.047); Limb salvage was 71.4% vs. 54.2% (HR
0.57 95% CI 0.24-1.35 p=0.203) and overall survival was 71.4%
vs. 33.3% (HR 0.37 95% CI 0.168–0.817 p=0.14).
Conclusion:
In our cohort the important clinical outcomes
following bypass surgery for chronic limb threatening ischemia
are far better if patients were enrolled in a local graft surveillance
protocol.
Recent Publications
1. Davies A H, Hawdon
A J, Sydes M R and
Thompson A G
(2005) Is Duplex
surveillance
of
value after leg vein
bypass
grafting?
C i r c u l a t i o n
112:1985-1991.
2. Hawdon A J, et al. (2003) Vein graft surveillance: is the
yield worth the effort? Acta Chir Belg 103:379-382.
3. Baril D T and Marone L K (2012) Duplex evaluation
following femoropopliteal angioplasty and stenting:
criteria and utility of surveillance. Vascular and
Endovascular Surgery 46:353-357.
4. Bui T D, Mills J L Sr, et al. (2012) The natural history
of duplex detected stenosis after femoropopliteal
endovascular therapy suggests questionable clinical
utility of routine duplex surveillance. Journal of Vascular
Surgery 55:346–352.
5. Abu Dhabri A M, Mohammed K, et al. (2017) Systemic
review and meta-analysis of duplex ultrasound
surveillance for infrainguinal vein bypass grafts. Journal
of Vascular Surgery 66:1885-1891.
Biography
Sanjay Singh has his expertise and passion in Vascular and Endovascular
Surgery. He has done complex aortic endovascular fellowship and is a Vas-
cular Consultant working in United Kingdom. His open and contextual surgi-
cal techniques are based on researched and practiced models which helped
to create new pathways for innovation. He has achieved this aptitude after
years of experience in research and teaching in university hospitals and insti-
tutions. The ever-responsive and adapting field of Endovascular Surgery has
improved the survival rates of high risk patients
dr_sanjaysingh@hotmail.comDoes duplex surveillance after femoro-popliteal bypass
grafting affect long term graft patency?
Sanjay Singh, Rushmi Purmessur
and
Arun Nair
Heart of England NHS Foundation Trust, UK
Sanjay Singh et al., J Vasc Endovasc Therapy 2018, Volume 3
DOI: 10.21767/2573-4482-C1-002