ISSN : ISSN: 2576-1455
Journal of Heart and Cardiovascular Research
Volume-outcome relationship in surgical aortic valve replacement for patients with aortic valve stenosis:a retrospective analysis of administrative data
Takeshi Umegaki1, Susumu Kunisawa1, Yasufumi Nakajima2, Takahiko Kamibayashi1, Kiyohide Fushimi1 and Yuichi Imanaka3*
1Department of Anesthesiology, Kansai Medical University Hospital, Osaka, Japan
2Department of Healthcare Economics and Quality Management, Graduate School of Medicine, Kyoto University, Kyoto, Japan
3Department of Health Policy and Informatics, Tokyo Medical and Dental University Graduate School, Tokyo, Japan
- *Corresponding Author:
- Yuichi Imanaka
Department of Healthcare Economics and Quality Management
Kyoto University Graduate School of Medicine
Yoshida Konoecho, Sakyoku, Kyoto, Japan
Tel: +81-75-753-4454
Fax: +81-75-753-4455
E-mail: imanaka-y@umin.net
Received Date: 29 September 2017; Accepted Date: 17 October 2017; Published Date: 26 October 2017
Citation: Umegaki T, Kunisawa S, Nakajima Y, Kamibayashi T, Fushimi K, et al. (2017) Volume-Outcome Relationship in Surgical Aortic Valve Replacement for Patients with Aortic Valve Stenosis: A Retrospective Analysis of Administrative Data. J Heart Cardiovasc Res. Vol. 2 No. 1: 109.
Copyright: © 2017 Umegaki T, et al. This is an open-access article distributed under the terms of the creative Commons attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The volume-outcome relationship between isolated surgical aortic valve replacement (SAVR) and mortality in patients with aortic valve stenosis remains unclear. This study aimed to assess this relationship using a large-scale study conducted in Japan. Methods: We conducted a retrospective cohort study of adult patients with aortic valve stenosis hospitalized between April 1, 2012 and March 31, 2015. Hospitals were categorized into 3 groups based on SAVR volume: low volume (≤49 cases), intermediate volume (50–99 cases), and high volume (≥100 cases). A multiple logistic regression analysis was performed with in-hospital mortality as the dependent variable and hospital volume groups as independent variables. Results: The low-volume group, intermediate-volume group, and high-volume group comprised 7383 patients from 330 hospitals, 5253 patients from 76 hospitals, and 3411 patients from 23 hospitals, respectively. The regression analysis accounted for patient sex, height, weight, activities of daily living, and comorbidities as covariates. Relative to the intermediate-volume group, the odds ratios for in-hospital mortality were 1.32 (95% confidence intervals: 1.07–1.61; P<0.01) in the low-volume group and 0.65 (0.48–0.87; P<0.01) in the high-volume group. Conclusion: Higher hospital volume was significantly associated with reduced mortality, and patients with aortic valve stenosis may benefit from care in high-volume hospitals.
Keywords
Volume-outcome relation; Surgical aortic valve replacement; Aortic valve stenosis; In-hospital mortality; Administrative data
Introduction
The number of surgeries for valvular heart disease in Japan has increased by 73.8% over the past decade [1]. There were 877 cases of transcatheter aortic valve implantation (TAVI) and approximately 10 000 cases of isolated surgical aortic valve replacement (SAVR) conducted in 2014, indicating that the latter accounted for the vast majority of aortic valve replacement surgeries [1].
The Diagnosis Procedure Combination (DPC) system is a patient case-mix system that was introduced in Japan in 2004, and has since become the prevalent method of payment for acute care hospitals. Under this system, hospitals produce and submit administrative data to insurers for the purpose of reimbursement. The data include patient information and itemized records of daily medical care, such as the types of medical tests, medications, and procedures provided to each patient, as well as the use of intensive or specialized care and nursing services. Information on procedures such as mechanical ventilation, renal replacement therapy, and the use of vasoactive agents are also available from DPC data, and previous studies have reported on the close association between these procedures and mortality [2-7]. Due to the extensive amount of information provided, DPC data has considerable potential for applications in healthcare research.
The first analysis of volume-outcome relationships in healthcare by Luft et al. in 1979 reported that mortality decreased with increasing surgical volume for several types of surgeries [8]. In an analysis of the volume-outcome relationship in SAVR by Patel et al. surgical volume was defined not only for SAVR, but also included procedures for ascending aorta and other valvular heart diseases [9]; that study reported that in-hospital and 30-day mortality rates decreased with increasing surgical volume. Astor et al. [10] analyzed the relationship between SAVR hospital volume and in-hospital mortality, and noted similar results to those of Patel et al. [9] Despite these studies, little is known about the volumeoutcome relationship between isolated SAVR procedures and in-hospital mortality.
In this study, we used Japanese DPC data to analyze hospital volume of isolated SAVR and SAVR with coronary artery bypass grafting (CABG) in patients with aortic valve stenosis to examine the volume-outcome relationship in SAVR unaccompanied by other valvular surgery.
Methods
Study design and data source
We conducted a retrospective multi-center cohort study of patients with aortic valve stenosis who had undergone SAVR at Japanese acute care hospitals between April 1, 2012 and March 31, 2015. All data were extracted from a DPC database comprising hospital administrative data collected by the DPC Research Group. Funded by the Ministry of Health, Labour and Welfare, the DPC Research Group conducts analyses using administrative data with the objective of further understanding and improving healthcare in Japan. The study was approved by the institutional ethics committee of Kansai Medical University Hospital (Approval number: H160404). This study was registered in the UMIN Clinical Trials Registry (UMIN-CTR) system (No. UMIN 000024725).
Patient selection
We first identified patients diagnosed with aortic valve stenosis who had undergone SAVR during the study period. Aortic valve stenosis was identified using the following International Classification of Diseases, 10th Revision codes: I060 (rheumatic aortic stenosis), I350 (nonrheumatic aortic stenosis), and I352 (nonrheumatic aortic stenosis with insufficiency). SAVR was identified using the K-code (used in DPC data to designate surgical procedures) K5551, which indicates valve replacement surgery. We excluded patients who were aged below 20 years, as well as those who had undergone aortic valvuloplasty, other valvular surgery at the same time as SAVR, or aortic root replacement. Patients who had undergone SAVR with CABG were included in analysis.
Patient characteristics
We collected information on the following patient baseline characteristics: age, sex, height, weight, activities of daily living (ADL) score at admission and discharge, Charlson comorbidity index, and New York Heart Association (NYHA) functional classification.
ADL scoring was based on 10 items with a maximum score of 20 points; the items were feeding (0–2 points), transferring (0–3 points), grooming (0–1 point), toileting (0–2 points), bathing (0–1 point), walking on level ground (0–3 points), climbing stairs (0–2 points), dressing (0–2 points), bowel continence (0–2 points), and urinary continence (0–2 points). Although the Charlson comorbidity index initially developed by Charlson et al. in 1987 has been widely used as a severity score for predicting 1-year mortality [11], this study used the modified comorbidity index developed by Quan et al. [12] Postoperative care was also analyzed using the number of days of mechanical ventilation after surgery and vasopressor use, as well as the proportions of patients who had undergone intraaortic balloon pumping (IABP), percutaneous cardiopulmonary support (PCPS), and tracheotomy.
Outcome measures
The main outcome measure used in this study was inhospital mortality. Other outcome measures included length of intensive care unit stay, length of hospital stay (overall stay, preoperative stay, and postoperative stay), and discharge destination (home, other hospital, nursing home, death, or others).
We also analyzed the incidence of the following postoperative complications: reoperation, emergency thoracotomy, hemorrhagic complications (excluding cerebral hemorrhage), cerebral infarction, cerebral hemorrhage, cardiac tamponade, and infection.
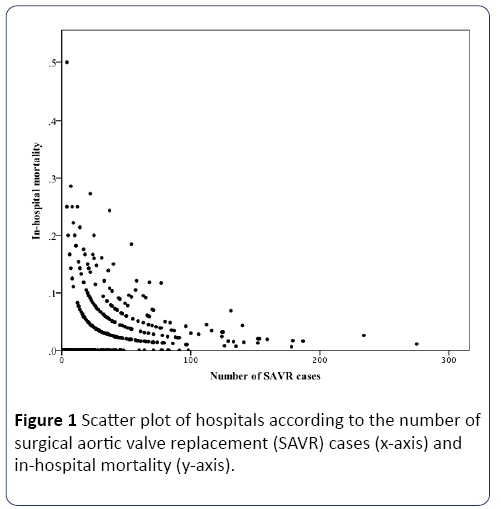
Statistical analysis
Continuous variables were calculated as means and standard deviations, and categorical variables were calculated as percentages. Based on the distribution of SAVR volume presented in Figure 1, hospitals were categorized into 3 groups designated the low-volume group (≤ 49 cases), intermediatevolume group (50–99 cases), and high-volume group (≥ 100 cases). To compare continuous variables among the 3 groups, we employed a non-repeated one-way analysis of variance with Tukey’s multiple comparison test. Categorical variables were analyzed using the Chi-square test. Patient characteristics were first examined using univariate analysis to identify those that had a significant relationship with inhospital mortality. These factors were then included as covariates in a multiple logistic regression analysis with inhospital mortality as the dependent variable and hospital volume (reference: intermediate-volume group) as the main independent variable of interest. The odds ratios (ORs) for the independent variables were calculated.
Results
The patient characteristics are presented in Table 1. The low-volume group, intermediate-volume group, and highvolume group comprised 7383 patients from 330 hospitals, 5253 patients from 76 hospitals, and 3411 patients from 23 hospitals, respectively. The mean ages of the patients in the 3 groups were similar at 75 years, but the other variables demonstrated significant inter-group differences. Although hospitals are required to provide information on the majority of these variables, the inclusion of information on NYHA classification is discretionary. As a result, there was a general lack of input for NYHA functional classification at 25.2%, 21.6%, and 26.8% for the low-, intermediate-, and high-volume groups, respectively. From the available information, the proportion of NYHA Class III and Class IV patients was low at 21.0% in the high-volume group; in contrast, the corresponding proportion was substantially higher at 37.9% in the low-volume group.
Table 1 Patient characteristics and outcomes (n=16 047).
| Variables | Low volume (n=7383) |
Intermediate volume (n=5253) |
High volume (n=3411) |
P value |
|---|---|---|---|---|
| Number of hospitals | 330 | 76 | 23 | |
| Patient characteristics | ||||
| Age (years) | 75.1±8.3 | 75.0±8.6 | 75.2±8.5 | 0.43 |
| Male (%) | 46.5 | 44.5 | 44.0 | 0.02 |
| Height (cm) | 153.1±17.4 | 152.1±20.9 | 152.4±18.5 | 0.02 |
| Weight (kg) | 55.2±11.9 | 54.4±12.5 | 55.0±11.8 | <0.01 |
| ADL score at admission | 18.0±5.1 | 18.4±4.5 | 18.4±4.3 | <0.01 |
| ADL score at discharge | 18.6±3.6 | 18.6±3.8 | 18.4±3.8 | 0.03 |
| Charlson comorbidity index (%) | ||||
| 0 | 50.0 | 56.1 | 55.6 | <0.001 |
| 1 | 16.0 | 16.4 | 15.3 | |
| 2 | 24.6 | 19.3 | 21.3 | |
| 3 | 6.7 | 5.8 | 5.8 | |
| ≥4 | 2.8 | 2.4 | 2.0 | |
| NYHA functional class (%) | ||||
| I | 14.2 | 14.5 | 18.0 | <0.001 |
| II | 47.9 | 44.5 | 61.1 | |
| III | 25.1 | 27.4 | 14.5 | |
| IV | 12.8 | 13.6 | 6.5 | |
| Procedure | ||||
| Isolated SAVR | 75.6 | 72.9 | 70.1 | <0.001 |
| Combined CABG and isolated SAVR | 24.4 | 27.1 | 29.9 | |
| Postoperative care | ||||
| Mechanical ventilation after surgery (days) | 2.6±5.9 | 2.5±5.6 | 2.2±5.3 | <0.001 |
| Use of vasopressor (days) | 3.1±4.4 | 2.9±4.6 | 2.6±3.8 | <0.001 |
| Renal replacement therapy (%) | 9.8 | 10.1 | 9.4 | 0.50 |
| Intra-aortic balloon pumping (%) | 5.5 | 6.1 | 3.2 | <0.001 |
| Percutaneous cardiopulmonary support (%) | 1.1 | 1.1 | 0.8 | 0.40 |
| Tracheotomy (%) | 1.9 | 1.7 | 1.3 | 0.10 |
| Outcomes | ||||
| ICU stay (days) | 4.2±4.0 | 4.3±3.7 | 3.7±3.4 | <0.001 |
| Overall hospital stay (days) | 36.7±31.2 | 34.5±27.8 | 28.5±19.8 | <0.001 |
| Preoperative hospital stay (days) | 8.3±13.4 | 7.7±13.2 | 7.3±19.1 | <0.01 |
| Postoperative hospital stay (days) | 27.4±28.9 | 25.8±26.9 | 20.2±24.5 | <0.001 |
| Discharge destination (%) | ||||
| Home | 83.5 | 78.2 | 77.9 | <0.001 |
| Other hospital | 11.2 | 17.5 | 19.5 | |
| Nursing home | 0.4 | 0.2 | 0.1 | |
| Death | 4.4 | 3.6 | 2.2 | |
| Other | 0.6 | 0.6 | 0.3 | |
| In-hospital mortality (%) | 4.4 | 3.6 | 2.2 | <0.001 |
Note:Values are presented as mean±standard deviation for continuous variables and number (percentage) for categorical variables. NYHA functional classification values were taken from the following sample sizes: low volume, n=1865; intermediate volume, n=1135; and high volume, n=913. Abbreviations: ADL, activities of daily living; CABG, coronary artery bypass grafting; ICU, intensive care unit; NYHA, New York Heart Association; SAVR, surgical aortic valve replacement
Despite the numerically similar duration of postoperative mechanical ventilation among the 3 groups (2.2-2.6 days), the analysis detected a statistically significant difference. The mean duration of vasopressor use in the high-volume group was 2.6 days, which was significantly lower than the lowvolume group (3.1 days) and intermediate-volume group (2.9 days). IABP use was also significantly less prevalent in the highvolume group relative to the other 2 groups. While PCPS use was also lower in the high-volume group, the difference was not statistically significant.
In-hospital mortality was observed to reduce as volume increased, with the mortality rates in the low, intermediate, and high-volume groups at 4.4%, 3.6%, and 2.2%, respectively. The mean overall length of hospital stay ranged from 28.5 days to 36.7 days across the groups, and the mean postoperative length of stay ranged from 20.2 to 27.4 days; the length of stay in the high-volume group was significantly shorter than in the other groups. In all 3 groups, the majority of patients were discharged to home, and those discharged to nursing homes comprised less than 0.5% of patients.
The proportions of postoperative complications are presented in Table 2. The analysis found significant differences in reoperation (P<0.01), hemorrhagic complications (excluding cerebral hemorrhage) (P<0.001), cerebral infarction (P<0.001), and infection (P<0.04). With the exception of hemorrhagic complications, the incidence of each complication in the highvolume group was lower than in the low-volume group.
Table 2 Complications after surgery (n=16 047).
| Postoperative complications | Low volume (n=7383) |
Intermediate volume (n=5253) |
High volume (n=3411) |
P value |
|---|---|---|---|---|
| Reoperation (%) | 7.5 | 6.9 | 5.8 | <0.01 |
| Emergency thoracotomy (%) | 1.8 | 1.7 | 1.6 | 0.82 |
| Hemorrhagic complications (excluding cerebral hemorrhage) (%) | 28.6 | 26.2 | 33.1 | <0.001 |
| Cerebral infarction (%) | 3.2 | 3.0 | 1.9 | 0.001 |
| Cerebral hemorrhage (%) | 0.2 | 0.2 | 0.1 | 0.36 |
| Cardiac tamponade (%) | 1.7 | 1.4 | 1.3 | 0.42 |
| Infection (%) | 9.0 | 9.6 | 8.0 | 0.04 |
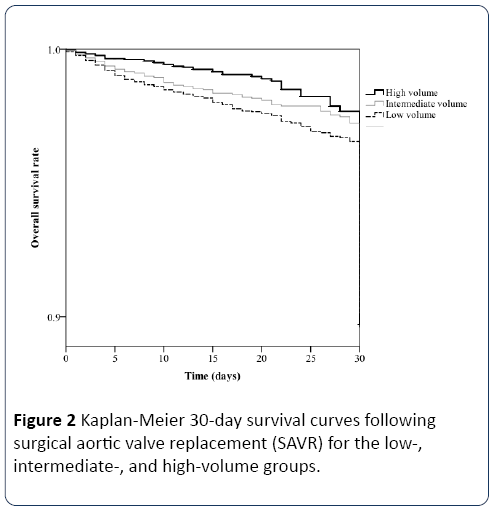
Table 3 shows the results of the multiple logistic regression analysis. Using the intermediate-volume group as the reference, the ORs for in-hospital mortality were 1.32 (95% confidence intervals: 1.07–1.61; P<0.01) in the low-volume group and 0.65 (95% confidence intervals: 0.48–0.87; P<0.01) in the high-volume group. Figure 2 shows the Kaplan-Meier survival curves until 30 days after SAVR. The log-rank test revealed a significant difference between the low- and highvolume groups (P<0.01).
Table 3 Results of multiple logistic regression analysis for in–hospital mortality in all cases (n=16 047).
| Variables | Odds ratio | 95% CI | P value |
|---|---|---|---|
| SAVR volume (reference: Intermediate volume) |
|||
| Low volume | 1.32 | 1.07–1.61 | <0.01 |
| High volume | 0.65 | 0.48–0.87 | <0.01 |
| Male | 1.30 | 1.07–1.58 | <0.01 |
| Height | 0.99 | 0.99–1.00 | 0.18 |
| Weight | 0.99 | 0.98–0.99 | <0.01 |
| ADL score at admission | 0.93 | 0.92–0.94 | <0.001 |
| Charlson comorbidity index (reference: 0) | |||
| 1 | 2.49 | 1.98–3.14 | <0.001 |
| 2 | 1.11 | 0.86–1.44 | 0.42 |
| 3 | 2.17 | 1.58–2.97 | <0.001 |
| ≥4 | 3.78 | 2.58–5.54 | <0.001 |
| Combined CABG and isolated SAVR (reference: isolated SAVR) | 1.88 | 1.57–2.26 | <0.001 |
Abbreviations: ADL, activities of daily living; CABG, coronary artery bypass grafting; CI, confidence intervals; SAVR, surgical aortic valve replacement
We also conducted a sub-analysis limited to the cases that included NYHA functional classification as covariates in the multiple logistic regression model (Table 4). With the inclusion of these variables, the analysis did not demonstrate a significant volume-outcome relationship.
Table 4 Results of multiple logistic regression analysis for in–hospital mortality limited to cases with NYHA coding (n=4220).
| Variables | Odds ratio | 95% CI | P value |
|---|---|---|---|
| SAVR volume (reference: Intermediate volume) |
|||
| Low volume | 1.30 | 0.83–2.03 | 0.26 |
| High volume | 1.01 | 0.56–1.85 | 0.96 |
| Male | 0.78 | 0.51–1.20 | 0.26 |
| Height | 0.99 | 0.98–1.00 | 0.11 |
| Weight | 1.01 | 0.99–1.03 | 0.36 |
| ADL score at admission | 0.97 | 0.95–1.00 | 0.04 |
| Charlson comorbidity index (reference: 0) | |||
| 1 | 2.03 | 1.12–3.67 | 0.02 |
| 2 | 0.93 | 0.55–1.59 | 0.79 |
| 3 | 1.49 | 0.80–2.78 | 0.22 |
| ≥4 | 4.37 | 2.23–8.58 | <0.001 |
| NYHA functional class (reference: I) | |||
| II | 1.16 | 0.47–2.87 | 0.75 |
| III | 4.36 | 1.83–10.44 | 0.001 |
| IV | 8.02 | 3.24–19.87 | <0.001 |
| Combined CABG and isolated SAVR (reference: isolated SAVR) | 1.92 | 1.29–2.85 | 0.001 |
Abbreviations: ADL, activities of daily living; CABG, coronary artery bypass grafting; CI, confidence intervals; NYHA, New York Heart Association; SAVR, surgical aortic valve replacement
Discussion
This study is the first to report on the volume-outcome relationship focused on isolated SAVR for aortic valve stenosis and in-hospital mortality. An important finding of this study was that hospital volume of the SAVR procedure itself had a significant relationship with the outcome of interest. Aortic valve stenosis is a serious condition that, in its natural course, often results in patient death within 2 to 5 years after the onset of symptoms [13]. As a result, aortic valve replacement procedures can be crucial for improving patient prognosis. Although previous studies have addressed volume-outcome relationships for SAVR [9,10], our study is characterized by the focus on isolated SAVR through the exclusion of other valvular or aortic surgeries. Our findings corroborate those of previous analyses, and reinforce our understanding of the volumeoutcome relationship in the SAVR procedure itself.
Recent studies from the US that assessed the volumeoutcome relationship in TAVI have reported significant associations between increasing volume and decreasing mortality [14,15]. However, TAVI was approved for insurance coverage in Japan only recently in October 2013, and there were as few as 877 TAVI procedures conducted in 20141. Although the short period of utilization and the small number of cases in Japan preclude analysis of the volume-outcome relationship in TAVI at present, this topic should be addressed in the future. Nevertheless, the results of this study and previous studies on valve replacement surgeries (both SAVR and TAVI) for aortic valve stenosis suggest that increases in surgical volume would likely result in reductions in mortality in the Japanese setting.
The use of administrative data, such as in this study and the report by Astor et al. [10], enables the implementation of large-scale multi-center analyses. An epidemiological research report in 2014 by the Japanese Association for Thoracic Surgery noted that the in-hospital mortality rate for patients who had undergone their first aortic valve replacement procedure was 2.4%, and the corresponding rate for SAVR patients with a previous history of aortic valve replacement surgery was 9.4% [1]. Our findings for in-hospital mortality were within this range. The studies by Jamieson et al. and Astor et al. report the 30-day mortality rates associated with isolated SAVR and SAVR with CABG to be approximately 4% and 8%, respectively [10,16]. In our analysis, the in-hospital mortality rates associated with isolated SAVR and SAVR with CABG were approximately 2.9% and 6.0%, respectively. As the length of hospital stay was approximately 30 days in our study sample, the mortality rates appear to be similar to those previously reported, and the slightly higher survival in our sample may be indicative of recent advances in therapy.
The DPC database does not allow for the follow-up of patients after discharge from hospital. The majority of patients were discharged home, with fewer than 20% and 0.5% of patients discharged to other hospitals and nursing homes, respectively. This finding is indirectly supported by previous studies that have reported that the health-related quality of life after aortic valve replacement is equal to or higher than the quality of life before surgery, therefore allowing for more patients to be discharged home [17-24]. The length of hospital stay was substantially longer in our study than in a previous study from the US [9]. The underlying reason for the relatively long hospitalizations in Japan is that acute care hospitals have traditionally also provided sub-acute and long-term care [25]. Recently, however, acute care hospitals have been under pressure from the Japanese government to reduce hospital stay durations. Admittedly, the protracted hospital stay durations in Japanese acute care hospitals allow for longer postoperative tracking, therefore enabling observations on short-term prognoses on a relatively large scale. Our findings do not provide any insight on long-term prognoses.
Our analysis found that the incidence of hemorrhagic complications (excluding cerebral hemorrhage) in the highvolume group was significantly higher than in the low-volume group. However, these results contradict the results on mortality, indicating that a large proportion of hemorrhagic complications were non-fatal. Sezai et al. conducted a singleinstitutional analysis of major adverse cardiovascular and cerebrovascular events (MACCE) in post-SAVR patients aged 80 years and older [26]. The study reported MACCE incidence to be 34.7%, and the incidences of cerebral infarction and cerebral hemorrhage were 1.3% and 2.7%, respectively. These incidences were generally higher than in our study sample, and the difference is likely due to the longer study period in Sezai et al. (our study was limited to the hospitalization period). It is possible that the significantly lower incidences of reoperation, cerebral infarction, and infection in the highvolume group are associated with the observed improvements in patient prognosis. Future studies should examine if there are also volume-outcome relationships with these outcomes.
A limitation of this study is the lack of input for NYHA functional classification. Despite the utility of NYHA classes as indicators of disease severity in patients with heart disease, hospitals are not required to include this information in DPC data. Due to the low quantity of input (approximately 25%), we were unable to incorporate this variable into the main multiple logistic regression analysis. Increases to the level of input on NYHA functional classifications would likely bring about changes to the relative proportions of NYHA classes within each group. However, we had included patient ADL scores and Charlson comorbidity index in the analysis to complement the assessment of each patient’s general condition. The second limitation is the lack of echocardiogram information, which did not allow us to examine ejection fractions or to conduct quantitative/qualitative assessments of the aortic valve. According to guidelines published by the American College of Cardiology and the American Heart Association in 2014, aortic valve replacement is a Class I recommended therapy for symptomatic and asymptomatic patients with severe aortic stenosis that have a left ventricular ejection fraction below 50% and are undergoing cardiac surgery for other indications [27]. Therefore, the lack of echocardiogram information precluded the assessment of SAVR from this perspective. The third limitation is the lack of clarity regarding therapy objectives and the cause of death. The administrative data do not indicate if renal replacement therapy was given for chronic or acute renal failure, or for a non-renal indication. Similarly, it is not clear if antihypotensive agents were used to treat hypovolemic or septic shock. In addition, the DPC system does not require hospitals to record the cause of death. We were therefore unable to determine if a patient had died due to surgery-related complications or for other reasons. The fourth limitation is the possibility that there may be factors that affect in-hospital mortality that were not included in our covariates. For example, we were unable to collect information on each patient’s surgical history. The noninclusion of such factors may have influenced our findings.
This study is, to the best of our knowledge, the first to observe a significant volume-outcome relationship focused on isolated SAVR. The large-scale multi-center analysis showed that increased hospital volume was significantly associated with reduced in-hospital mortality. Patients with aortic valve stenosis may benefit from care in high-volume hospitals, and future research should address the possible deficiencies in low-volume institutions.
Conflict of Interest
The authors declare no conflicts of interest, financial or otherwise.
Acknowledgements
This study was supported in part by a Health and Labour Sciences Research Grant from the Ministry of Health, Labour and Welfare, Japan (Grant Number: H27-iryo-ippan-001, H28- seisaku-sitei-009) and a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (Grant number: [A] 16H02634).
References
- Masuda M, Okumura M, Doki Y, Endo S, Hirata Y, et al. (2016) Thoracic and cardiovascular surgery in Japan during 2014: Annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 64: 665-697.
- Terblanche M, Adhikari NK (2006) The evolution of intensive care unit performance assessment. J Crit Care 21: 19-22.
- Lin YF, Ko WJ, Chu TS, Chen YS, Wu VC, et al. (2009) The 90-day mortality and the subsequent renal recovery in critically ill surgical patients requiring acute renal replacement therapy. Am J Surg 198: 325-332.
- Brar H, Olivier J, Lebrun C, Gabbard W, Fulop T, et al. (2008) Predictors of mortality in a cohort of intensive care unit patients with acute renal failure receiving continuous renal replacement therapy. Am J Med Sci 335: 342-347.
- Soubrier S, Leroy O, Devos P, Nseir S, Georges H, et al. (2006) Epidemiology and prognostic factors of critically ill patients treated with hemodiafiltration. J Crit Care 21: 66-72.
- Pinsky MR (2007) Hemodynamic evaluation and monitoring in the ICU. Chest 132: 2020-2029.
- Lundberg GD (1994) Practice parameter for the use of fresh-frozen plasma, cryoprecipitate, and platelets. JAMA 271: 777-781.
- Luft HS, Bunker JP, Enthoven AC. (1979) Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med 301: 1364-1369.
- Patel HJ, Herbert MA, Drake DH, Hanson EC, Theurer PF, et al. (2013) Aortic valve replacement: using a statewide cardiac surgical database identifies a procedural volume hinge point. Ann Thorac Surg 96: 1560-1565.
- Astor BC, Kaczmarek RG, Hefflin B, Daley WR. (2000) Mortality after aortic valve replacement: results from a nationally representative database. Ann Thorac Surg 70: 1939-1945.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373-383.
- Quan H, Li B, Couris CM, Fushimi K, Graham P, et al. (2011) Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173: 676-682
- Ross J, Braunwald E (1968) Aortic stenosis. Circulation 38: 61-67.
- Kim LK, Minutello RM, Feldman DN, Swaminathan RV, Bergman G, et al. (2015) Association between transcatheter aortic valve implantation volume and outcomes in the United States. Am J Cardiol 116: 1910-1915.
- Badheka AO, Patel NJ, Panaich SS, Patel SV, Jhamnani S, et al. (2015) Effect of hospital volume on outcomes of transcatheter aortic valve implantation. Am J Cardiol 116: 587-594.
- Jamieson WR, Edwards FH, Schwartz M, Bero JW, Clark RE, et al. (1999) Risk stratification for cardiac valve replacement. National Cardiac Surgery Database. Database Committee of The Society of Thoracic Surgeons. Ann Thorac Surg 67: 943-951.
- Shan L, Saxena A, McMahon R, Wilson A, Newcomb A (2013) A systematic review on the quality of life benefits after aortic valve replacement in the elderly. J Thorac Cardiovasc Surg 145: 1173-1189.
- Sundt TM, Bailey MS, Moon MR, Mendeloff EN, Huddleston CB, et al. (2000) Quality of life after aortic valve replacement at the age of >80 years. Circulation 102: III70-74.
- Vicchio M, Della Corte A, De Santo LS, DeFeo M (2008) Tissue versus mechanical prostheses: Quality of life in octogenarians. Ann ThoracSurg 85: 1290-1295.
- Ennker J, Dalladaku F, Rosendahl U, Ennker IC, Mauser M, et al. (2006) The stentless freestyle bioprosthesis: impact of age over 80 years on quality of life, perioperative, and mid-term outcome. J Card Surg 21: 379-385.
- Lam BK, Hendry PJ (2004) Patients over 80 years: quality of life after aortic valve replacement. Age Ageing 33: 307-309.
- Spaziano M, Carrier M, Pellerin M, Choiniere M (2010) Quality of life following heart valve replacement in the elderly. J Heart Valve Dis 19: 524-532.
- Vicchio M, Della Corte A, De Feo M, Santarpino G, De Santo LS, et al. (2007) Quality of life after implantation of bileaflet prostheses in elderly patients: an anticoagulation work group experience. Ann ThoracSurg 84: 459-465.
- Vicchio M, De Santo LS, Della Corte A, De Feo M, Provenzano R, et al. (2008) Aortic valve replacement with 19-mm bileaflet prostheses in the elderly: left ventricular mass regression and quality of life. J Heart Valve Dis 17: 216-21.
- Ikegami N, Campbell JC (1995) Medical care in Japan. N Engl J Med 333: 1295-99.
- Sezai A, Osaka S, Yaoita H, Ishii Y, Arimoto M, et al. (2015) Early and Long-term outcomes in Japanese patients aged 80 years or older undergoing conventional aortic valve replacement. Ann ThoracCardiovascSurg 21: 247-253
- Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, et al. (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63: e57-185.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences