ISSN : 2573-0320
Journal of Transmitted Diseases and Immunity
Trends in HIV Prevalence among Pregnant Women in Lusaka Province, Zambia 1994-2008
Kasonde GM1*, Makasa M2 and Michelo C1
1Department of Epidemiology & Biostatistics, School of Public Health, The University of Zambia, Lusaka, Zambia
2Department of Community & Family Medicine, School of Public Health, The University of Zambia, Lusaka, Zambia
- *Corresponding Author:
- Kasonde GM
Department of Epidemiology & Biostatistics
School of Public Health, The University of Zambia
Lusaka, Zambia, P.O Box 370251, Kafue, Zambia
Tel: +260 21 1295220
E-mail: greatykasonde@gmail.com
Received date: April 26, 2018; Accepted date: June 12, 2018; Published date: June 09, 2018
Citation: Kasonde GM, Makasa M, Michelo C (2018) Trends in HIV Prevalence among Pregnant Women in Lusaka Province, Zambia 1994-2008. J Transm Dis Immun Vol.2 No.1:1
Abstract
Background: Human immunodeficiency virus infection can contribute to reduced maternal and child population based health outcomes. In certain regions of subSaharan Africa, new HIV infections have been reported to continue to rise in spite of PMTCT programs. We examined the trends of HIV prevalence among pregnant women aged 15-49 years attending antenatal care in Lusaka Zambia for the period 1994-2008. Methods: We conducted a retrospective cross sectional study on data nested on the six repeated national ANC sentinel surveillance cycles on HIV and syphilis at the four Lusaka sites namely, Chelstone, Chilenje, Kalingalinga and Matero. Pregnant women aged 15-49 years attending their first ANC clinic visit received syphilis testing as well as anonymous HIV testing. In this study we focused on the period 1994-2008 for Lusaka Province. All data analysis was conducted using Stata version 12.1. Logistic regression analysis was applied to assess the association between HIV infection and other predictor variables. Results: Overall 16,694 pregnant women were included in the study. HIV prevalence declined from 27.3% in 1994 to 24.1% in 2008 (P<0.001), contrasting differences by site and age group were observed. HIV prevalence was significantly lower in age group 15-24 years than the older age-groups (20.9% versus 32.1%, P-value <0.001). Site patterns showed that in Chelstone, HIV prevalence declined from 24.7% in 1994 to 20.9% in 2008 (P = 0.03), 35.3% to 24.2% (P<0.001) in Chilenje and from 28.4% to 24.4% (P=0.02) in Matero. In contrast, Kalingalinga recorded an increase from 21.7% to 26.7% (P<0.001) for the same period. HIV infection among pregnant women was associated with syphilis infection (aOR 2.12; 95%CI 1.67- 2.69). Conclusion: Overall HIV infection among pregnant women in Lusaka has declined over the years. The unchanging burden observed in selected age groups and site may suggest limitations of the PMTCT program in reaching these groups. The results of our study highlight the need to strengthen HIV prevention and control efforts to specific target groups.
Keywords
HIV; Prevalence; Trends; Pregnancy; Zambia
Background
It is more than 30 years now since the Human Immunodeficiency Virus (HIV) that causes Acquired Immunodeficiency Syndrome (AIDS) in humans was first detected, infecting approximately 75 million people in the world [1]. In 1994 the global total HIV infections exceeded 17 million [2]. By the year 2007, about 33 million people were infected with human immunodeficiency virus [3]. Since then, the epidemic has continued to claim many lives and more people are getting infected and about 36 million people have died. According to estimates by World Health Organization (WHO) and UNAIDS, globally, 19 million of the 35 million people living with HIV did not know that they had the virus in 2014 [1,4]. Surveillance of human immunodeficiency virus (HIV) infection among pregnant women attending antenatal care (ANC) has continued to be the mainstay system of monitoring the HIV epidemic in most countries of Sub-Saharan Africa [5,6].
Many studies reveal that model-based estimates of the global proportions of maternal deaths that are in HIV-infected women range from 7% to 21%, and the effect of HIV on the risk of maternal death is highly uncertain [7]. Another longitudinal study conducted in the sub Saharan Africa revealed that the mortality for HIV-infected pregnant women were approximately 8.0 times higher than HIV-uninfected counterparts. It is further predicted that 24% of deaths in pregnant women are attributable to HIV in Sub-Saharan Africa [8]. HIV/AIDS, could potentially complicate the target to meet SDG number 3 which aspires for healthy lives and promote well-being for all including a bold commitment to end the epidemics of AIDS/TB and other communicable diseases by 2030. It targets to reduces the global maternal mortality ratio to less than 70% per 100,000 live births and end preventable deaths of newborns and children under 5 years [9]. HIV/AIDS still contributes greatly to high child and maternal mortality and continues to cause poor maternal health in those that survive mortality thereby impeding the achievement of SDG 3 by 2030 [7].
If the impact of the prevention efforts are to be realized, the initial signs of this effect is supposed to be seen in the most affected groups. One way to generate this information is through examining patterns and trends of infection in the population including the most affected sub-populations notwithstanding the wide geographical and sub-population contrasts in infection burden that may exist. Such knowledge especially about setting specific HIV infection burden, trends and patterns is essential for general interventional planning, resource allocation and evaluating of prevention efforts [10]. Lusaka is the main city, and it is the most populated town in Zambia with an estimated population of 2.3 million. Demographic health surveys have also shown that the city has had one of the highest HIV burden [11]. However the oldest data available even before the ZDHS was undertaken in 2001 was sentinel surveillance data collected since 1994. Despite this, critical analysis of the exact burden as well as patterns of HIV infection among ANC attendees in Lusaka has been limited and generally lumped in country pooled estimates. This information could have been a critical barometer on the understanding of the infection pattern in Zambia in urban areas which historically were most affected. In addition, this could have been a pointer on how well the response against HIV (such as PMTCT, Counseling and Testing as well as ART in general) is performing given that in such a city, resources may be more available and better accessed than in most other places with similar HIV infection burden [6]. However, the HIV infection pattern among pregnant women attending Lusaka ANC has not been adequately examined making it difficult to use that information to examine on whether the response on HIV infection is going in the right direction. Thus, in this study we aimed at determining the HIV prevalence and possible determinants among pregnant women aged 15-49 years attending antenatal care in selected Lusaka urban sites for the period 1994-2008.
Methods
Design
We carried out a retrospective cross sectional study based on the data nested on the repeated national ANC sentinel surveillance of HIV and Syphilis in Zambia. The study involved pregnant women aged 15-49 years who attended ANC in Lusaka at any of the sentinel surveillance site during the period of data collection. Four ANC urban sites which are also among the most urbanized and highly populated part of the city with the population of 2.3 million, include Chelstone, Chilenje, Kalingalinga, and Matero [6]. All pregnant women attending antenatal care for the first time for that pregnancy from any the four ANC sentinel surveillance sites and accepted routine syphilis testing and anonymously tested for HIV comprised the de facto eligible population and were included in the analysis. In these sentinel surveys, the target is a sample size of about 500 women per site for a period of four months [12].
Data extraction
Data for the four sites extracted included all socio demographic information as well as data on HIV test and syphilis test results. These results originate from the blood specimens obtained from eligible women tested for both HIV-1/2 and syphilis from the local laboratory during the surveys. The specimens for HIV testing were anonymous and unlinked to the women. Capillus HIV-1/2 (Cambridge diagnosis. UK) was the first test for screening HIV for the period 1994-2008 surveys and all reactive specimens were re tested using confirmatory tests wellcozyme HIV. Discordant specimen results were re tested using tie breakers, Bionor HIV- 1/2 (Bionor AS, Norway). Quality control and confirmatory testing was done by two national reference laboratories, that is tropical diseases research center (TDRC) in Ndola for the Northern region and the University teaching hospital (UTH) virology laboratory in Lusaka for the Southern region [13]. A more detailed data collection and description of the ANC sentinel surveillance system in Zambia has been reported elsewhere [5,14-18]. For this study, all data that had complete records of HIV infection and for the four urban sites in Lusaka Province were extracted for final analysis.
Statistical Analysis
Data analysis was conducted using Stata (STATACORP, version 12.1, College Station, Texas, USA). HIV prevalence estimates and the associated trends tests for each site were calculated using the mantel- hanszel chi- square (X2) for trend. All factors that were considered as priori confounders were analysed at univariate one by one. Log binomial regression was used to estimate the relative risk of HIV infection by the socio- demographic characteristics and Syphilis exposure. Multiple logistic regression was employed to control for confounders with level of statistical significance at 95% confidence level p-value <0.05. To find a best fit model, a generalized investigator led stepwise backward regression model was used excluding factors one at a time until the remaining factors were statistically significant (P-value <0.05).
Results
Population characteristics
Between 1994 and 2008 six HIV sentinel surveys had been conducted. A total of 16792 women received antenatal services in the period under review, but only 16694 (de facto final sample) were in the age category 15-49 and eligible for inclusion in the study. From the six HIV sentinel surveys conducted, the overall site sample size of pregnant women who received antenatal services and were tested for HIV was 4156 in Cheltone, 4613 in Chilenje, 3938 in Kalingalinga, and Matero reported 4085. The median age of pregnant women who participated in the surveys was 24 years.
HIV infection burden
The overall HIV prevalence for the period under study was 26% whereas the prevalence by site over time was 28.9% in Matero, 26.3% in Kalingalinga, 26.6% in Chilenje and 23.1% in Chelstone. Table 1 also shows the characteristics of the pregnant women that participated in HIV sentinel surveillance. Pregnant women who reported that they live in rural areas, 20.5% were HIV positive with odds ratio 0.73 (95% CI 0.59-0.91) verses 26.5% of those who reported living in urban areas were HIV positive. Showing that women in rural areas are less likely to have HIV than those from urban areas (Table 2). Rural residence was then understood to be the peripheral slums from among the unplanned settlements. HIV prevalence was significantly different by age groups with regard to self-reported residence. Younger women (15-19 years) who reported to reside in urban areas had lower HIV prevalence than those from the rural 15.7% versus 16.1% respectively. From the urban area, 495 were HIV positive women representing 15.7% pregnant women in the age group 15- 19 years were HIV positive against 23.8% that was observed among women aged 20-24 years, P-value <0.001 odds ratio 1.71 (95% CI 1.52-1.92). The highest HIV prevalence observed was 34.4.% among women aged 30-39 years p-value <0.001 with odds ratio 2.82 (95% CI 2.49-3.21). in the rural area, women aged 15-19 years had lower HIV prevalence than older age groups but the differences were not statistically significant p- value >0.05.
Table 1:HIV prevalence and socio-demographic characteristic of pregnant woman by residence (1994–2008)
| Residence | |||||||
|---|---|---|---|---|---|---|---|
| Urban | Rural | ||||||
| Social demographic | Overall HIV prevalence n (%) | HIV prevalence n (%) | P_value | OR(95% CI) | HIV prevalence n (%) | P_value | OR(95% CI) |
| Age category; (years) | |||||||
| 15-19 | 495 (15.6) | 459(15.7) | ref | 36(16.1) | ref | ||
| 20-24 | 1394 (23.8) | 1,319(24.1) | <0.001 | 1.71(1.52-1.92) | 75(20.8) | 0.162 | 1.37(0.9-2.1) |
| 25-29 | 1357 (32.1) | 1,289(32.9) | <0.001 | 2.64(2.34-2.97) | 68(22.0) | 0.094 | 1.47(0.9-2.2) |
| 30-39 | 1016 (33.2) | 961(34.4) | <0.001 | 2.82(2.49-3.21) | 55(21.2) | 0.161 | 1.39(0.9-2.2) |
| 40-49 | 40 (17.7) | 35(17.5) | 0.489 | 1.14(0.78-1.67) | 5(20.0) | 0.623 | 1.30(0.5-3.7) |
| Number of School years | |||||||
| 0-6 | 775 (22.6) | 675 (23.0) | ref | 100(20.2) | ref | ||
| 7 | 1097(27.6) | 1,030(28.5) | <0.001 | 1.34(1.20-1.50) | 67(19.2) | 0.729 | 0.94(0.7-1.3) |
| 9-Aug | 1145 (27.6) | 1,105(28.0) | <0.001 | 1.30(1.17-1.46) | 40(21.2) | 0.771 | 1.06(0.7-1.6) |
| 11-Oct | 373 (30.8) | 362(31.1) | <0.001 | 1.51(1.30-1.76) | 11(25.6) | 0.401 | 1.36(0.7-2.8) |
| ≥ 12 | 848 (24.3) | 827(24.5) | 0.158 | 1.09(0.97-1.22) | 21(23.3) | 0.494 | 1.21(0.7-2.1) |
| Educational level; | |||||||
| Primary | 1,872 (25.3) | 1,705(26.0) | ref | 167(19.8) | ref | ||
| Secondary | 1,518 (28.3) | 1,467(28.7) | 0.001 | 1.14(1.05-1.24) | 51(22.0) | 0.456 | 1.14(0.80-1.6) |
| Tertiary | 848 (24.4) | 827(24.7) | 0.094 | 0.92(0.85-1.01) | 21(23.3) | 0.422 | 1.24 (0.74-2.1) |
| Number of months pregnant | |||||||
| 1st trimester | 695 (27.3) | 663(27.6) | ref | 32 (24.8) | ref | ||
| 2nd trimester | 2,677 (25.7) | 2,525(26.1) | 0.155 | 0.93(0.84-1.03) | 152(20.7) | 0.295 | 0.79(0.51-1.2) |
| 3rd trimester | 441 (24.6) | 390(25.4) | 0.14 | 0.90(0.78-1.04) | 51(19.9) | 0.272 | 0.75(0.46-1.3) |
| Last pregnancy outcome | |||||||
| live birth | 2955 (17.2) | 2,774(29.1) | ref | 181(21.6) | ref | ||
| still birth | 94 (28.5) | 91(39.7) | 0.001 | 1.61(1.23-2.10) | 3(10.0) | 0.139 | 0.40(0.12-1.3) |
| abortion | 189 (36.3) | 181 (34.7) | 0.006 | 1.30(1.08-1.56) | 9(18.4) | 0.59 | 0.82(0.39-1.7) |
| 1st pregnancy | 516 (33.3) | 501 (17.4) | <0.001 | 0.51(0.46-0.57) | 15(12.6) | 0.025 | 0.52(0.30-0.9) |
| Syphilis. | |||||||
| No | 3925 (25.1) | 3,706(25.6) | ref | 219(19.6) | ref | ||
| Yes | 370 (40.6) | 343(41.2) | <0.001 | 2.04(1.77-2.35) | 27(35.1) | 0.002 | 2.21(1.36-3.6) |
| Marital status. | |||||||
| married | 2,524 (26.2) | 2,408(26.8) | ref | 116 (18.2) | ref | ||
| separated/divorced | 81 (34.6) | 78(34.4) | 0.011 | 1.43(1.09-1.89) | 3(42.9) | 0.115 | 3.37(0.74-15.3) |
| widowed | 17 (44.7) | 15(41.7) | 0.048 | 1.95(1.01-3.80) | 2(100) | ----------- | -------------------- |
| single | 268 (19.0) | 259(19.0) | <0.001 | 0.64(0.56-0.74) | 9(20.9) | 0.656 | 1.20(0.56-2.6) |
| Numberof pregnancies | |||||||
| primigravid | 1,065 (19.9) | 1,013(20.1) | ref | 52(18.5) | ref | ||
| multigravid | 2,655 (30.0) | 2,514(30.6) | <0.001 | 1.75(1.61-1.91) | 141(22.5) | 0.179 | 1.28(0.89-1.8) |
| grandgravid | 562 (24.6) | 511(25.6) | <0.001 | 1.37(1.21-1.55) | 51(17.9) | 0.851 | 0.96(0.63-1.5) |
| Number of months since last gave birth | |||||||
| 1st pregnancy | 637 (17.8) | 598(17.9) | ref | 39(18.1) | ref | ||
| 24-Jan | 701 (27.6) | 651(28.5) | <0.001 | 1.83(1.61-2.08) | 50(19.7) | 0.653 | 1.11(0.70-1.8) |
| 25-36 | 732 (24.6) | 670(25.0) | <0.001 | 1.53(1.35-1.74) | 62(20.8) | 0.439 | 1.19(0.76-1.9) |
| 37-60 | 790 (28.3) | 744(29.0) | <0.001 | 1.90(1.65-2.11) | 46 (21.8) | 0.333 | 1.27(0.79-2.0) |
| 61-120 | 564 (41.2) | 548 (42.1) | <0.001 | 3.33(2.90-3.84) | 16(23.2) | 0.348 | 1.37(0.71-2.7) |
| ≥ 121 | 86 (52.1) | 78(51.7) | <0.001 | 4.90(3.52-6.83) | 8(66.7) | 0.001 | 9.08(2.60-31.7) |
| Number of children ever had | |||||||
| 1st pregnancy | 965 (19.2) | 906 (19.2) | ref | 59(20.6) | ref | ||
| 3-Jan | 2,390(30.3) | 2,258(30.9) | <0.001 | 1.88(1.72-2.05) | 132(22.6) | 0.509 | 1.12(0.80-1.6) |
| 6-Apr | 431(25.8) | 394(27.0) | <0.001 | 1.56(1.36-1.78) | 37 (17.5) | 0.388 | 0.82(0.52-1.3) |
| 9-Jul | 27(16.9) | 23 (18.1) | 0.752 | 0.93(0.59-1.47) | 4(12.5) | 0.28 | 0.55(0.19-1.6) |
| 10/more | 5(23.8) | 2(18.2) | 0.93 | 0.93(0.20-4.33) | 3(30.0) | 0.478 | 1.65(0.41-6.6) |
HIV prevalence trends among pregnant women (1994-2008)
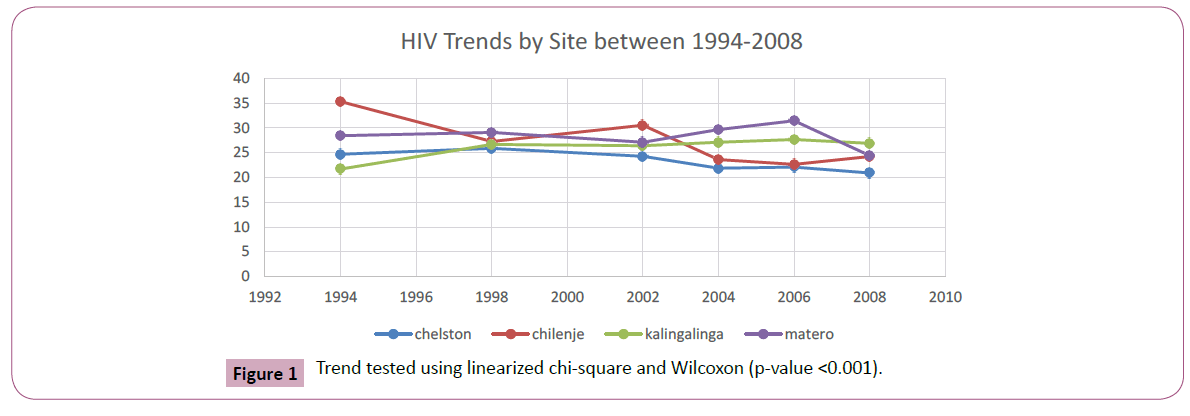
Table 2a shows HIV prevalence trends and the odds ratio for changes in HIV prevalence for all sites among pregnant women aged 15-49 years for the period 1994-2008. The trend was tested using the linearized chi-square with p value <0.001. In 1994, 1824 pregnant women participated in the sentinel surveillance for HIV in Lusaka province and 27.3% were HIV positive. HIV prevalence remained steadily high at 27% up to 2002. In 2004 we observed some decline in HIV prevalence from 27.1% in 2002 to 25.6% aOR. 0.89(95% CI 0.78-1.02), however, this was not statistically significant. The decline continued to 2008, 3,294 pregnant women participated in the survey and 24.1 % were HIV positive. This was statistically significant with adjusted odds of 0.77 (95%CI 0.67-0.88). This decline in HIV prevalence is illustrated in Figure 1 below.
Table 2a: HIV Prevalence trend for Lusaka province; 1994-2008.
| ANC survey year | n(%) | OR | p-value | 95%CI | *OR | p-value | 95%CI* |
|---|---|---|---|---|---|---|---|
| 1994 | 498 (27.3) | ref | ref | ||||
| 1998 | 628 (27.0) | 0.99 | 0.847 | 0.86-1.13 | 1 | 0.962 | 0.87-1.16 |
| 2002 | 801 (27.1) | 0.99 | 0.893 | 0.87-1.13 | 0.98 | 0.796 | 0.86-1.12 |
| 2004 | 773 (25.6) | 0.92 | 0.186 | 0.80-1.04 | 0.89 | 0.084 | 0.78-1.02 |
| 2006 | 846 (25.8) | 0.93 | 0.246 | 0.81-1.05 | 0.87 | 0.032 | 0.76-0.99 |
| 2008 | 794 (24.1) | 0.85 | 0.012 | 0.74-0.96 | 0.77 | <0.001 | 0.67- 0.88 |
*Adjusted “Age as categorical variable”.
n _ number of participants (HIV+).
Ref _ reference
Table 2b shows HIV prevalence trends and the odds ratio at 95% confidence level by site and year of sentinel surveillance. From the table, it clearly shows that HIV prevalence among pregnant women has continued to decline since 2002. In chelston 24.7% pregnant women were HIV positive in 1994 and in 2002 it was 24.3%. It reveals that it declined to 21.9% in 2004 and 20.9% in 2008. The decline was not showing enough evidence before adjusting for age category, aORs 0.73 (95% CI 0.55-0.097). The decline was much more clear in Chilenje, which reveals that in 1994 HIV prevalence was 35.3% declined to 24.2% in 2008. This decline was not by chance we can rule out chance finding, both at unadjusted and adjusted levels. Adjusting for age category reveals that the decline in HIV prevalence could be as low as 32% to as high as 59% with probability 95% from the population and its statistically significant p_value <0.001. The other site in which substantial HIV prevalence among pregnant women declined was observed in Matero. In 1994, 28.4% pregnant women were HIV positive in Matero. Despite the decline being gradual, HIV prevalence reduced to 24.4% in 2008 and this was statistically significant controlling for age category aORs 0.72 (95% CI 0.54- 0.95). In 1994, HIV prevalence in Kalingalinga was 21.7% this raised to 26.7% in 2008 and it was very much unstable over the years. However, there was not enough evidence to this effect controlling for age category aORs 1.26 (0.97-1.65). Figure 1 illustrates HIV prevalence trends by site and sentinel surveillance year.
Table 2b: HIV prevalence trends odds ratio and 95% confidence interval by site and survey year (15-49 years).
| ANC survey year & site | n(%) | p-value | OR | 95%CI | *OR | P value | 95%CI* |
|---|---|---|---|---|---|---|---|
| Chelston | |||||||
| 1994 | 114 (24.68) | ref | ref | ||||
| 1998 | 210 (25.86) | 0.64 | 1.07 | 0.82-1.39 | 1.12 | 0.404 | 0.86-1.47 |
| 2002 | 191 (24.27) | 0.872 | 0.98 | 0.75-1.28 | 0.97 | 0.8 | 0.73-1.27 |
| 2004 | 162 (21.86) | 0.259 | 0.85 | 0.65-1.12 | 0.83 | 0.195 | 0.63-1.10 |
| 2006 | 219 (22.08) | 0.272 | 0.87 | 0.67-1.12 | 0.8 | 0.101 | 0.61-1.04 |
| 2008 | 167 (20.90) | 0.121 | 0 .81 | 0.62-1.06 | 0.73 | 0.028 | 0.55-0.97 |
| Chilenje | |||||||
| 1994 | 161 (35.31) | ref | ref | ||||
| 1998 | 139 (27.25) | 0.007 | 0.69 | 0.52- 0.90 | 0.68 | 0.006 | 0.51-0.90 |
| 2002 | 241 (30.54) | 0.084 | 0.81 | 0.63-1.03 | 0.78 | 0.051 | 0.62-1.01 |
| 2004 | 187 (23.61) | <0.001 | 0.57 | 0.44-0.73 | 0.54 | <0.001 | 0.42-0.70 |
| 2006 | 158 (22.64) | <0.001 | 0.54 | 0.41-0.70 | 0.5 | <0.001 | 0.38-0.65 |
| 2008 | 217 (24.22) | <0.001 | 0.59 | 0.46- 0.75 | 0.53 | <0.001 | 0.41-0.68 |
| Kalingalinga | |||||||
| 1994 | 111 (21.68) | ref | ref | ||||
| 1998 | 133 (26.65) | 0.065 | 1.31 | 0.98-1.75 | 1.39 | 0.028 | 1.04-1.87 |
| 2002 | 156 (26.40) | 0.069 | 1.3 | 0.98-1.71 | 1.33 | 0.049 | 1.01-1.77 |
| 2004 | 187 (27.10) | 0.032 | 1.34 | 1.03-1.76 | 1.38 | 0.023 | 1.05-1.81 |
| 2006 | 220 (27.64) | 0.016 | 1.38 | 1.06-1.80 | 1.34 | 0.032 | 1.03-1.75 |
| 2008 | 215 (26.88) | 0.034 | 1.33 | 1.02-1.73 | 1.26 | 0.086 | 0.97-1.65 |
| Matero | |||||||
| 1994 | 112 (28.43) | ref | ref | ||||
| 1998 | 146(29.08) | 0.829 | 1.03 | 0.77-1.38 | 1.01 | 0.96 | 0.75-1.37 |
| 2002 | 213(27.10) | 0.63 | 0.94 | 0.72-1.23 | 0.93 | 0.598 | 0.71-1.22 |
| 2004 | 237(29.66) | 0.659 | 1.06 | 0.81-1.39 | 1.01 | 0.93 | 0.77-1.33 |
| 2006 | 249(31.44) | 0.288 | 1.16 | 0.89-1.51 | 1.08 | 0.565 | 0.83-1.42 |
| 2008 | 195(24.41) | 0.135 | 0.81 | 0.62-1.07 | 0.72 | 0.019 | 0.54-0.95 |
*Age adjusted as categorical variable.
n _ proportion per site. % _ HIV prevalence
Ref _reference.
Associated factors
The main factors associated with infection were age, educational attainment, residence, and syphilis infection. The proportion of women who attained at least primary education were significantly higher in urban than rural areas; (26.0% Vs. 19.8% respectively, P<0.001). The HIV positivity rate among women with secondary level education was 28.7% with odds of 1.14 this was statistically significant at 95% (CI 1.05-1.24) in urban area and 22.0% in rural area with odds 1.14 (95% CI 0.80-1.6). It has been observed that 25.3% women with primary level of education and 28.3% with secondary education were HIV positive regardless of their residence. Those with secondary level of education were 1.17 times more likely to have HIV than those with primary education, this was statistically significant at 95% confidence level (CI 1.08- 1.26). we further observed that women with tertiary level of education were less likely to have HIV than those with primary education. However this observation was not statistically significant OR 0.95 95% (CI 0.87-1.04) (Table 3).
Table 3: Predictor variables of HIV among pregnant women in all the four sites in Lusaka (1994-2008).
| univariate | Multivariate | |||
|---|---|---|---|---|
| Predictor variable | n(%) | P-value | OR95% Cl | AOR95%Cl |
| Age categoriry | ||||
| 15-19 | 496 (15.6) | ref | ref | |
| 20-24 | 1399 (23.8) | <0.001 | 1.69 (1.51-1.89) | 1.61 (1.33-1.96) |
| 25-29 | 1363 (32.1) | <0.001 | 2.55 (2.27-2.86) | 2.42 (1.96- 2.99) |
| 30-39 | 1021 (33.2) | <0.001 | 2.68 (2.37-3.02) | 2.66 (2.13-3.34) |
| 40-49 | 40 (17.7) | 0.412 | 1.16 (0.81-1.65) | 1.40 (0.87-2.25) |
| Number of pregnancies | ||||
| primigravid | 1,067 (19.9) | ref | ||
| multigravid | 2,668 (30.0) | <0.001 | 1.73 (1.59-1.87) | |
| grandgravid | 564 (24.6) | <0.001 | 1.31 (1.17- 1.47) | |
| Marital status | ||||
| married | 2,538 (26.2) | ref | ref | |
| separated/divorced widowed | 81 (34.6) | 0.004 | 1.49 (1.14-1.96) | 2.68 (1.54- 4.68) |
| single | 17 (44.7) | 0.012 | 2.28 (1.20- 4.33) | 2.20 (1.03- 4.70) |
| 268 (19.0) | <0.001 | 0.66 (0.57-0 .76) | 1.09(0.91-1.29) | |
| Last pregnant outcome | ||||
| live birth | 518 (17.2) | ref | ref | |
| still birth | 94 (28.5) | 0.006 | 1.43 (1.11-1.85) | 1.57 (1.07-2.32) |
| abortion | 191 (36.3) | 0.013 | 1.26 (1.05-1.50) | 1.50(1.15-1.97) |
| no prev preg (1st child) | 518 (33.3) | <0.001 | 0.52 (0.47-0.58) | 1.51(0.79-2.89) |
| Syphilis | ||||
| No | 3941 (25.1) | ref | ref | |
| Yes | 373 (40.6) | <0.001 | 2.04 (1.78- 2.34) | 2.12 (1.67- 2.69) |
| Residence | ||||
| Urban | 4,074 (26.5) | ref | ref | |
| Rural | 246 (20.5) | <0.001 | 0.71 (0.62-0.83) | 0.73 (0.59-0.91) |
| Number of months pregnant | ||||
| 1=1st trimester | ||||
| 2=2nd trimester | 697 (27.3) | ref | ||
| 3=3rd trimester | 2,690 (25.7) | 0.099 | 0.92 (0.84-1.02) | |
| 443 (24.6) | 0.049 | 0.87 (0.76-0.999) | ||
| Number of yrs in school | ||||
| 0-6 | 780 (22.6) | ref | Ref | |
| 7 | 1101(27.6) | <0.001 | 1.31 (1.18-1.45) | 1.25 (1.07-1.46) |
| 9-Aug | 1149 (27.6) | <0.001 | 1.31 (1.18-1.45) | 1.39 (1.20-1.61) |
| 11-Oct | 373 (30.8) | <0.001 | 1.52 (1.32- 1.76) | 1.60 (1.30-1.97) |
| ≥ 12 | 852 (24.3) | 0.083 | 1.10 (0.99-1.23) | 1.03 (0.87-1.20) |
| Number of months since last gave birth | ||||
| 1st pregnancy | 639 (17.8) | ref | ref | |
| 24-Jan | 705 (27.6) | <0.001 | 1.76 (1.56-1.99) | 1.85 (0.98-3.49) |
| 25-36 | 736 (24.6) | <0.001 | 1.50 (1.34-1.70) | 1.64 (0 .86-3.14) |
| 37-60 | 792 (28.3) | <0.001 | 1.82 (1.61-2.05) | 1.82 (0.95-3.44) |
| 61-120 | 569 (41.2) | <0.001 | 3.38 (2.81-3.70) | 3.00 (1.56-5.73) |
| ≥ 121 | 86 (52.1) | <0.001 | 5.02 (3.65- 6.89) | 5.95 (2.84-12.4) |
| Educational level; | ||||
| Primary | 1,881 (25.3) | ref | ||
| Secondary | 1,522 (28.3) | <0.001 | 1.17 (1.08-1.26) | |
| Tertiary | 852 (24.4) | 0.29 | 0.95 (0.87-1.04) | |
| Number of children ever had | ||||
| 1st pregnancy | 967 (19.2) | ref | ||
| 3-Jan | 2,403(30.3) | <0.001 | 1.83 (1.68-1.99) | |
| 6-Apr | 433(25.8) | <0.001 | 1.46 (1.28-1.67) | |
| 9-Jul | 27(16.9) | 0.46 | 0.85 (0.56-1.30) | |
| 10/more | 5(23.8) | 0.595 | 1.31 (0.48-3.60) |
Among the HIV positive women who reported in the first trimester 27.6% were from the urban, while the rural women 24.8%. In the second trimester, 26.1% of women who reported to reside in urban areas were HIV positive and 20.7% was observed among women in rural areas (Table 1). Few women had their first ANC visit in the third trimester in both urban and rural areas. Reviewing the outcome of the last pregnancy among the women shows that there were more women with HIV in urban area who reported to have still birth or abortion. 39.7% of women had still birth and 34.7% had abortion in urban areas while in rural area 10.0% had still births and 18.4% had abortion as shown in Table 1. Table 3 shows that 28.5% women who had still births were HIV positive and the odds of 1.57 at 95% CI (1.07-2.32), this was statistically significant. 36.3% women who had abortion were HIV positive with odds of 1.50 at 95% CI(1.15-1.97). We also observed that in women who were having their first pregnancy, 33.3% were HIV positive unadjusted odds ratio 0.52 95% CI (0.47-0.58).
When we examined the association of HIV and syphilis among women, it was observed that women who had syphilis were more likely to have HIV with the odds of 2.12 times than that among women with no syphilis infection regardless of their educational attainment, marital status, and residence. Women in urban areas who had syphilis were 2.04 time more likely to have HIV and those in rural areas had slight higher chances of having HIV than those in urban areas with the odds of 2.21 times than that among women with no syphilis infection. Further, 40.6% of women who had positive syphilis results were also HIV positive. 25.1% were HIV positive but had no syphilis while 59.4% had only syphilis positive results. Exploring HIV prevalence and marital status among the women in the study revealed that, HIV prevalence was higher among women who reported to be widowed and those who were on separation or divorced, this was both among women in urban and rural areas as shown in Table 1 below. Exploring this further, 34.6% women who were on separation or divorced were HIV positive. This was statistically significant with the odds of 2.68 at 95% CI (1.54- 4.68). We observed that 44.7% of widows were HIV positive with the odds of 2.20 at 95% CI (1.03- 4.70). 26.1% married women were HIV positive and the least HIV prevalence was observed among singles at 19.0% with unadjusted odds ratio 0.66 95% CI (0.57-0 .76) (Table 3)
Discussion
The study reveals that HIV prevalence had substantially declined during the period from 2002 to 2008 although there were marked differentials by age, educational attainment and geolocation. The finding that HIV infection burden increased with age was similar to the findings from other studies conducted in Zambia and the region and this may be attributed to changing biological attributes correlated with higher need for sexual pleasures [14,15]. This was also similar to the finding of the study conducted in Brazil among 54139 pregnant women who received antenatal HIV screening from a network of public healthcare centers in 2011 which revealed that HIV prevalence was higher in the older age groups. In this population, the burden of HIV infection seems to be concentrated in lower educated groups (primary and secondary level of education) and the presence of syphilis doubled this burden.
Further, HIV infection burden was heavier in married women than singles as already demonstrated in previous studies in this country [5,14]. It has been revealed that widowed women are 2.2 times more likely to have HIV than married women. The study further reveals that women who are on separation or divorced are more likely to have HIV than married women. The reasons for these differentials are unclear and were beyond the scope of this study. However we believe that some of these may be linked to the influence of various interventional programs aimed to reduce heterosexual transmission such as PMTCT, the abstanance, be faithful and use a condom (ABC) strategy as well as rolled out counselling and testing campaign [3,19,20]. One could further argue that unless a couple knows their HIV status, the likelihood of unprotected sex is logically the norm, making transmission possible. This is plausible in these settings largely because HIV testing and condom use especially with casual partners is still low [16]. This could also explain why we observed high HIV prevalence among married women.
There was a strong positive perfect correlation between HIV and syphilis infection among pregnant women and this finding confirms earlier observations from examining the entire country data [17]. Accordingly Syphilis increase the risk of HIV infection, and has been associated with increased viral load and a reduction in CD4 count in individuals dually infected [7,17].
The study revealed that pregnant women who had still births and abortion had increased chances of HIV than those who had live births previously. This was similar to the study conducted by [18,19] on the impact of HIV 1 on fertility in sub-Saharan Africa, causes and consequences. Despite Lusaka being an urban area, self-reported residence by women in the study revealed higher HIV prevalence among pregnant women in urban areas than those in rural areas and this was similar to the findings from other studies conducted in the region [20-22]. Except for single women in rural areas who had higher HIV prevalence than their single counterparts in urban areas. The decline in HIV prevalence in women suggest that the response to intervention measures introduced by the MOH and other co-operating partners had been positive.
The overall HIV prevalence in Kalingalinga, a site showing unchanging burden over time, showed an increase in HIV prevalence. The reasons for this are unclear and were beyond the scope of this study although there is anecdotal information suggesting that this trend could be due to the high internal migration to this area. This could result to selection bias, with the effect of unequal attrition from which more women infected with HIV migrate to this area. We have revealed substantial decline in HIV prevalence in Chelstone. In 1994, Chelstone recorded 24.7%, since that time Chelstone has recorded a continuous decline in HIV prevalence among women accessing ANCs. However and in contrast, Kalingalinga shows a contrasting picture. These site differentials observed suggests the presence of critical differences and clustering of populations according to risk even when geo-locations are comparable like in this case.
Limitation and Strength of the Study
Several biases associated with HIV sentinel designs have been described already. . Firstly, wide coverage of the surveillance program, coupled with some rotation in personnel supervisors, makes it difficult to keep the standard operating procedure comparable over subsequent years. Secondly, it was usually assumed that the ANC group was representative of all pregnant women although this may not be the case. This may not be true in Lusaka also, since poor women are more likely to use ANCs in public health facilities than private clinics if at all. Further, others have argued that the women participating in all the HIV and Syphilis sentinel survey and in this case since 1994, is an exposed group thereby making a higher likelihood for overestimation of HIV prevalence in this population. However,. We argue that sentinel surveillance data is meant to examine trends and not point estimates, hence repetitive cross sectional studies among pregnant women with similar characteristics, is a norm, thereby giving a picture of what is happening in the population over time. We therefore conclude that the results from this study can be generalized with extrapolations of overall HIV prevalence only as far as trends of HIV infection are concerned. Secondly, examining these patterns in a capital city where interventions are likely to be concentrated also gives a crude indication on the influence and performance of preventive programs.
Conclusion
HIV infection among pregnant women in Lusaka has substantially declined over the years overall. The unchanging burden observed in selected age groups and site may suggest limitations of the PMTCT program in reaching these groups. This calls for a need to strengthen prevention and control efforts to target these groups and aim to incorporate effective syphilis control as it can potentially exacerbate HIV transmission and infection. Early ANC bookings in the first trimester should be encouraged and emphasized among pregnant women. This will enable early detection and treatment of HIV and other infections like syphilis to enhance PMTCT, reduce infant morbidity and mortality, and improve maternal health. A more recent HIV surveillance should be conducted in order to ascertain the course of HIV prevalence trend in Lusaka.
Competing Interests
There were no competing interests.
Authors' Contribution
GK participated in the conception of the study, acquisition of data, carried out the statistical analysis and drafted the manuscript. MM and CM reviewed all the drafts for intellectual content and participated in the interpretation of the findings and review of the manuscript. All authors read and approved the final manuscript.
Acknowledgement
The authors wish to thank all those who were involved in the data collection that made this study (dissertation) possible. Thanks to my supervisors Dr. Mpundu Makasa and Prof. Charles Michelo. Also not forgetting Dr. Patrick Musonda for the guidance in the statistical analysis using STATA Software and also Prof. Knut Fylkesnes for assistance on data acquisition and analysis. I would also like to acknowledge the support of the mentors; Mr. Mumbi Chola and Ms. Rosalia Dambe.
References
- World Health Organization Unaids, Unicef (2014) The global Health Sector strategy on HIV/AIDS 2011-2015, An interim review of progress; Geneva, Joint United Nations Program on HIV/AIDS.
- Merson MH (1994) Making AIDS prevention a national priority. Integration pp: 2-5.
- Hallett TB, Aberle-Grasse J, Bello G, Boulos lM, Cayemittes MPA, et al. (2006) Declines in HIV prevalence can be associated with changing sexual behaviour in Uganda, urban Kenya, Zimbabwe, and urban Haiti. Sex Transm Infect 82: 1-8.
- Karamisheva V, Ivanov S, Nachev A, Marinov B, Jordanova D, et al. (2013) [HIV infection in pregnant women and risk of preterm birth. Akusherstvo i ginekologiia 52: 21-4.
- Dzekedzeke K, Fylkesnes K (2006) Reducing uncertainties in global HIV prevalence estimates: the case of Zambia. BMC Public Health 6: 83.
- Central Statistical Office, Central Board of Health, Orc Macro, Zambia Demographic and Health Survey 2007. Calverton, Maryland: ORC Macro: 1-375.
- UNAIDS/WHO: "AIDS epidemic update: December 2014"special report on HIV prevention. Geneva, Joint United Nations Program on HIV/AIDS; 2014.
- Zaba B, Calvert C, Marston M, Isingo R, Nakiyingi-Miiro J, et al. (2013) Effect of HIV infection on pregnancy-related mortality in sub-Saharan Africa: secondary analyses of pooled community-based data from the network for Analysing Longitudinal Population-based HIV/AIDS data on Africa (ALPHA). Lancet 381: 1763-1771.
- World Health Organization, UNAIDS, UNDP (2015) The global Sustainable Development Goals (SDGs) 2030, interim paper progress; Geneva, Joint United Nations Program on HIV/AIDS.
- Stringer EM, Sinkala M, Kumwenda R, Chapman V, Mwale A, et al. (2004) Personal risk perception, HIV knowledge and risk avoidance behavior, and their relationships to actual HIV serostatus in an urban African obstetric population. Journal of acquired immune deficiency syndromes 35: 60-606.
- World Health Organization; Global Health Observatory (GHO) progress report; Geneva, Joint United Nations Program on HIV/AIDS; 2014; Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector.
- Fylkesnes K, Musonda RM, Kasumba K, Ndhlovu Z, Mluanda F, et al. (1997) The HIV epidemic in Zambia: socio-demographic prevalence patterns and indications of trends among childbearing women. PLoS One 8: e79189.
- Kayeyi N (2013) Trends in HIV Prevalence and Sexual Behaviour among Young People in Zambia; geographical and socio-economic differentials. University of Bergen press. Norway.
- NAC TDRC, SIDA, CDC, (2003) Zambia Antenatal Clinic Sentinel Surveillance Report 1994-2002. Lusaka Zambia National HIV/AiDS Council, Tropical Disease Research Center, Swedish International Development Cooperation Agency, and Center for Disease Control and Prevention.
- Michelo C, Sandøy IF, Dzekedzeke K, Siziya S, Fylkesnes K (2006) Steep HIV prevalence declines among young people in selected Zambian communities: population-based observations (1995–2003). Published: 10 November 2006. BMC Public Health 6: 279.
- Sandoy IF, Kvale G, Michelo C, Fylkesnes K (2006) Antenatal clinic-based HIV prevalence in Zambia: declining trends but sharp local contrasts in young women. Tropical Medicine & International Health: TM & IH 11: 917-28.
- Makasa M, Fylkesnes K, Michelo C, Kayeyi N, Chirwa B, et al. (2012) Declining syphilis trends in concurrence with HIV declines among pregnant women in Zambia: observations over 14 years of national surveillance. Sexually Transmitted Diseases 39: 173-81.
- Gregson Saj, Zaba B, Hunter S (2003) The impact of HIV 1 on fertility in sub-Saharan Africa: causes and consequences. United Nations Population Division.
- Buve A, Carael M, Hayes RJ, Auvert B, Ferry B, et al. (2001) Multicentre study on factors determining differences in rate of spread of HIV in sub-Saharan Africa: methods and prevalence of HIV infection. AIDS 15: S5-14.
- Bouare N, Gothot A, Delwaide J, Bontems S, Vaira D, et al. (2013) Epidemiological profiles of human immunodeficiency virus and hepatitis C virus infections in Malian women: Risk factors and relevance of disparities. World J Hepatology 5: 196-205.
- Kankasa C, Siwale M, Kasolo F, Nishiyama A, Terunuma H, et al. (2005) Socioeconomic and reproductive factors associated with condom use within and outside of marriage among urban pregnant women in Zambia. African J Reproductive Health 9: 128-36.
- Shan D, Sun J, Khoshnood K, Fu J, Duan S, et al. (2005) The impact of comprehensive prevention of mother-to-child HIV transmission in Dehong prefecture, Yunnan province, 2005-2010: A hard-hit area by HIV in Southern China. Inter J STD AIDS.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences