Paraspinal Compartment Syndrome in a Teenage Athlete
Jyoti Sharma1*, Elizabeth Kiselak1, Javier Perez1, Saraswati Dayal1, Sanjeev Kaul1 and Martin Karpeh2
1Department of Trauma and Surgical Critical Care, Hackensack Meridian Health Center, Hackensack, NJ, USA
2Department of Surgery, Hackensack Meridian Health Center, Hackensack, NJ, USA
- *Corresponding Author:
- Jyoti Sharma
Department of Trauma and Surgical Critical Care
Hackensack Meridian Health Center, Hackensack, NJ, USA
Tel: (551) 996-2900
E-mail: jyoti.sharma@hackensackmeridian.org
Received date: May 26 2018; Accepted date: June 7 2018; Published date: June 14 2018
Citation: Sharma J, Kiselak E, Perez J, Dayal S, Kaul S, et al. (2018) Paraspinal Compartment Syndrome in a Teenage Athlete. J Emerg Trauma Care Vol.3:No.1:4.
Abstract
Background: Acute paraspinal lumbar compartment syndrome was first described in the early 1980s as a rare entity. Similar to other types of compartment syndromes, early diagnosis and appropriate management has shown to improve functional outcomes. Current literature continues to highlight cases of non-operative management despite persistent clinical symptoms, rhabdomyolysis, muscle atrophy on MRI, and delayed return to exertional activities. Objective: Discuss the presentation, diagnosis, and management of acute lumbar paraspinal compartment syndrome. Case Report: A 15-year-old male presented with a four day history of persistent lower back pain and rhabdomyolysis after completing cross fit training. A magnetic resonance imaging (MRI) was obtained which demonstrated diffuse bilateral paraspinal musculature inflammation. The patient was noted to have bilateral paraspinal tenderness with focal paresthesia to the right paraspinal region. Despite aggressive fluid resuscitation, the creatine kinase (CK) remained elevated. Neurosurgery spine consultation was obtained and due to progressively worsening pain, the patient was taken to the operating room (OR) for bilateral paraspinal fasciotomies and debridement of devitalized muscle. Intraoperatively, right greater than left paraspinal muscle necrosis was noted. On postoperative day 2 (POD), the patient returned to the OR for closure of the fasciotomy sites with plastic surgery. Serial creatine kinase trended down and eventually normalized. The patient was discharged home with no functional deficits. Conclusion: Acute lumbar paraspinal compartment syndrome is a rare entity that should be considered in the differential diagnosis in young athletes presenting with unexpected lower back pain associated with severe rhabdomyolysis. Treatment involves muscle compartment release, possible muscle debridement, fluid resuscitation, and serial creatine kinase measurements.
Keywords
Oxide scale; Acute paraspinal compartment syndrome; Lumbar spine; Rhabdomyolysis; Fasciotomy
Introduction
In 1881, von Volkmann from Germany described the first case of compartment syndrome [1,2]. Compartment syndrome is an increased pressure within a closed fibro-osseous space that causes reduced blood flow and tissues perfusion [3]. If left surgically untreated, this may result in ischemia with muscle necrosis and irreversible damage to the tissues of the compartment [3]. Compartment syndrome has been reported in almost all anatomical areas of the extremities and the abdomen [2]. Acute lumbar paraspinal compartment syndrome is a rare entity often reported to occur after exertional activities such as skiing, weightlifting, surfing, and as a result of reperfusion injury during abdominal aortic injury [3,4]. To date, there are approximately twenty-three cases of this type of compartment syndrome cited in the literature, half of which were managed surgically [5].
In this case report, a young athlete presented to the emergency department with persistent paraspinal lower back pain and rhabdomyolysis requiring surgical fasciotomy.
Case Report
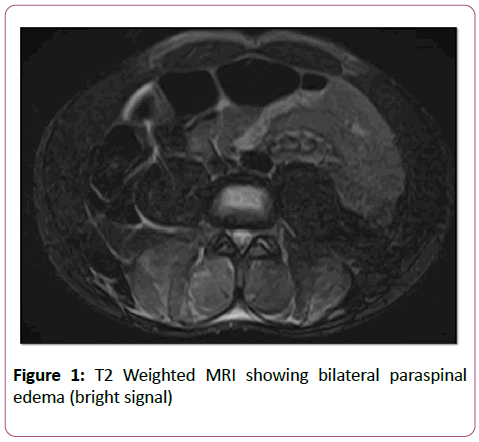
A 15-year-old male with no significant medical problems was transferred to our pediatric critical care unit (PICU) after being assessed at an outside hospital (OSH) for a complaint of severe lower back pain and rhabdomyolysis. The pain began 4 days prior, after the patient completed a cross fit training session with kettle bells. Two days later, the patient was seen by his primary care physician during which time he was treated with cyclobenzaprine without relief. The following day he was transported to an outside hospital where laboratory findings included a creatine kinase (CK) level of 78,000 IU/L. He was transferred to a second hospital for a higher level of care where his CK remained persistently elevated. A magnetic resonance imaging (MRI) showed an isolated finding of diffuse bilateral paraspinal musculature inflammation with some tracking fluid (Figure 1).
The patient was subsequently transferred to our institution for specialized care. Physical examination revealed bilateral paraspinal tenderness with focal paresthesia to the right paraspinal muscle area and no edema or ecchymosis (Figure 2). Despite aggressive fluid resuscitation, his CK remained elevated, greater than 38,000 IU/L. A neurosurgery spine specialist was consulted. Due to progressive worsening pain worrisome for compartment syndrome, the patient was taken to the OR for paraspinal compartment decompression.
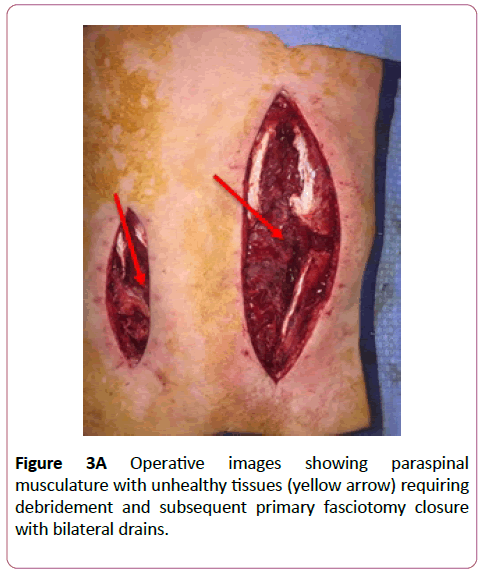
Intraoperatively, fluoroscopic localization of the spinal column was undertaken to prevent neurological complications.Paraspinal decompression was then performed by making a 5-8cm incision down through the skin and subcutaneous tissue along the vertical axis of each paraspinal muscles. Once encountered, the thoracolumbar fascia was incised and the paraspinal muscles released. There was severe right paraspinal muscle necrosis and mild left spinal muscle necrosis as indicated by dark, non-bleeding muscle in the middle and inferior aspect of the muscle bundle (Figure 3). A moderate amount of devitalized muscle was sharply debrided. Hemostasis was achieved and each wound was irrigated with saline and bilateral wound vacuum-assisted closure devices (V.A.C.™) were applied.
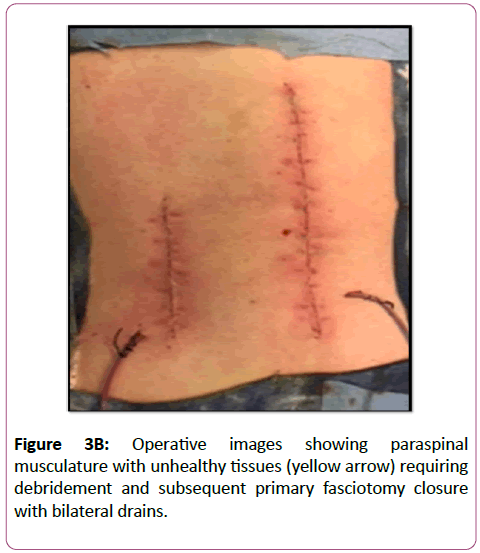
On Postoperative day 2 (POD), the patient returned to the OR during which time pulse irrigation and Versajet™ were used for micro-debridement of any remaining necrotic tissue. Adequate hemostasis was achieved with bovie electrocautery and thrombin injections. The plastic surgery team completed closure of the fasciotomy sites. Bilateral Blake drains were placed (Figure 3A and 3B).
Post-operatively, CK trended downward and eventually normalized. The patient participated in physical therapy and was able to ambulate with no gross restrictions. He was discharged home on POD 6 with no complications.
Discussion
Acute paraspinal compartment syndrome is a rare entity that requires a high index of suspicion for diagnosis. This syndrome can be classified into acute (Type I) or chronic (Type II) [2]. Type I subtypes include the following: atraumatic (Subtype A; downhill skiing, surf boarding, weight lifting), direct trauma (Subtype B), and secondary to non-spinal surgery (Subtype C; aortic bypass, gastric bypass) [2]. This patient presented with Type I, Subtype A lumbar paraspinal compartment syndrome.
Unlike extremity compartment syndrome where classical signs include pain, paresthesia, paresis, pallor, poikilothermia, and pulselessness, in acute paraspinal compartment syndrome all these symptoms are not appreciated [6]. Clinical presentation is typically with localized pain, tenderness, rigidity, and paresthesia [2,3,5]. Interestingly, patients may also have decreased or absent bowel sounds and activities that raise the intra-abdominal pressure may exacerbate symptoms [2,3].
Laboratory findings supporting the diagnosis include elevated creatine kinase (CK), urine myoglobin, creatinine, aspartate aminotransferase, and alanine aminotransferase [2,3,6]. Edema, inflammation, and/or hematoma on MRI usually identifies the paraspinal compartment [2,3,6]. Measuring of intra-compartment pressures confirms the diagnosis with pressures that are usually significantly elevated (70-80 mmHg) [2].
Once acute paraspinal compartment syndrome is suspected, management should focus on the following: aggressive resuscitation with intravenous fluids, avoidance of nephrotoxic drugs, cessation of any further traumatic activities, and urgent surgical decompression with fasciotomy [2,3,5]. Although conservative management with non-operative intervention is an option, patients have demonstrated improved outcomes with surgical fasciotomy even when it is delayed (for Type II) [2,5]. Improved outcomes include lack of paraspinal muscle atrophy and chronic back pain with exertional activities as well as a shorter time period to return to baseline function [2,5].
The patient described in this case report presented with symptoms, signs, laboratory values, and imaging (i.e., localized paraspinal tenderness, right-sided lower back paresthesia, persistently elevated CK with rhabdomyolysis, and an MRI showing paraspinal edema) suspicious for acute lumbar paraspinal compartment syndrome prompting surgical decompression with bilateral paraspinal fasciotomies. Early consideration of this rare entity for young athletes with lower back pain and unexplained rhabdomyolysis may prompt early surgical intervention, improved functional outcomes, and earlier return to exertional activities.
Conclusion
Acute lumbar paraspinal compartment syndrome is a rarity that should not only be considered in the differential diagnosis in young athletes presenting with unexpected lower back pain associated with severe rhabdomyolysis, but also prompt early operative intervention with fasciotomy.
References
- Volkmann RV (1881) Die ischamischen Muskellahmungen und kontracturen. Centralblatt fur Chirurgie, Leipzig.
- Nathan ST, Roberts CS, Deliberato D (2012) Lumbar paraspinal compartment syndrome. International Orthopedics 36: 1221-1227.
- Paryavi E, Jobin CM, Ludwig SC, Zahiri H, Cushman J, et al. (2010) Acute exertional lumbar parspoinal compartment syndrome 35: E1529-33.
- Chavez JM, Gonzalez PG (2013) Suspected lumbar compartment syndrome: A rare cause of low back pain after strenuous exercise. Spine J 13: 1409-1410.
- Alexander W, Low N, Pratt G (2018) Acute lumbar paraspinal compartment syndrome: A systemic review. ANZ J Surg.
- Mattiassich G, Larcher L, Leitinger M, Trinka E, Wechselberger G, et al. (2013) Paravertbral compartment syndrome after training causing severe back pain in an amateur rugby player: report of a rare case and review of the literature. BMC Musculoskelet Disord 14: 259.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences