Less Carbohydrate Intake Increases Serum Ketone Bodies in Low Carbohydrate Diet
Hiroshi Bando1,2*, Koji Ebe2,3, Takako Manabe4, Masahiro Bando5 and Yoshikazu Yonei6
1Tokushima University, Nakashowa, Tokushima, Japan
2Japan Low Carbohydrate Diet Promotion Association, Kyoto, Japan
4Kagawa Yoga Association, Kagawa, Japan
5Department of Nutrition and Metabolism, Institute of Biomedical Sciences, Tokushima University Graduate School, Tokushima, Japan
6Anti-Aging Medical Research Center, Graduate School of Life and Medical Sciences, Doshisha University, Kyoto, Japan
- *Corresponding Author:
- Hiroshi Bando, MD, PhD, FACP
Tokushima University
Nakashowa, Tokushima, Japan
Tel: +81-90-3187-2485
Fax: +81-88-603-1030
E-mail: pianomed@bronze.ocn.ne.jp
Received Date: 12 February 2018; Accepted Date: 16 March 2018; Published Date: 26 March 2018
Citation: Bando H, Ebe K, Manabe T, Bando M, Yonei Y (2018) Less Carbohydrate Intake Increases Serum Ketone Bodies in Low Carbohydrate diet. Endocrinol Metab Vol. 2 No.1: 109.
Copyright: © 2018 Bando H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Discussion has continued for Calorie Restriction (CR) and low carbohydrate diet (LCD). We have investigated clinical research of LCD in various states for years.
Case and results: The patient was 61 year-old female with HbA1c 10.5%, BMI 21.2 kg/m2 and normal vitals and physicals. Laboratory data were Hb 15.2 g/dl, Alb 5.0 g/dL, Triglyceride 43 mg/dL, HDL-C 89 mg/dL, LDL-C 152 mg/dL, immunoreactivity insulin (IRI) 2.9 μU/mL serum C-peptide reactivity (s-CPR) 1.0 ng/mL, total ketone bodies (T-KB) 3081 μmol/L (28-120), acetoacetic acid (AcAc) 300 μmol/L (14-68), 3-hydroxybutyric acid (3-OHBA) 2781 μmol/L (0-74) Autoantibodies were negative for Glutamate decarboxylase (GADA) or Islet cell (IA-2). She was diagnosed as type 2 diabetes mellitus (T2DM) and started super LCD formula meal with 12% of carbohydrate, and recorded carbohydrate amount about 20-40g per day. HbA1c value was 8.1% and 6.6% in 2 and 4 months, respectively. Significant relationship was shown between carbohydrate intake and hyperketonemia. AcAc/T-KB ratio was 15-20% and around 10%, when T-KB is less than 1000 μmol/L and more than 1000 μmol/L, respectively.
Discussion and conclusion: Authors have proposed 3 types of LCD, which are petit, standard and super, with 40%, 26%, 12% of carbohydrate ratio. Continuing super- LCD usually brings elevated ketone bodies, which might have beneficial function for maintaining the health and anti-aging medicine. Currently obtained results would become the fundamental data and suppose future directions and recommendations for research of ketone bodies in low carbohydrate diet.
Keywords
Low carbohydrate diet; Super low carbohydrate diet; 3-Hydroxybutyric acid; Acetoacetic acid; Ketone bodies; Hyperketonemia
Abbreviations
LCD: Low-Carbohydrate Diet; CR: Calorie Restriction; T2DM: Type 2 Diabetes Mellitus; VLCKD: Very Low-Carbohydrate Ketogenic Diet; 3-OHBA: 3- Hydroxybutyric Acid; IRI: Insulin Immunoreactivity; CPR: C-Peptide Reactivity
Introduction
Concerning the nutritional therapy, lots of discussion have been continued in comparison with Calorie Restriction (CR) and low carbohydrate diet (LCD). LCD has been originated by Atkins and Bernstein in western countries [1,2]. After that, LCD has been reported to have various clinical efficacy by several investigators [3-6]. Clinical efficacy of LCD for 2 years compared with CR and Mediterranean diet and similar efficacy for 4 years were shown [3,4]. Consecutively, several researchers reported clinical research of LCD in the light of various axes [5-7].
On contrast, in Japan, the authors firstly initiated LCD and reported the effect of LCD in clinical practice [8,9]. We proposed useful three kinds of LCD formula diet, which are super LCD, standard LCD and petit LCD, which have been clinically effective for patients with diabetes and metabolic disease and patients necessary to reduce weight [10,11]. With these clinical nutritional therapy, we have also developed social movement, continuing the activity of Japan LCD Promotion Association with lectures and journals.
Furthermore, we have investigated LCD in patients with various states including fetus-placenta-newborn-mother axis. We have reported the results that remarkable elevated ketone bodies are found in these axes, and that these findings would suggest the important roles of ketone bodies as an energy source [12,13].
The characteristic effect of LCD would be elevated level of ketone bodies in blood [14,15]. From the biochemical point of view, ketone bodies include three elements, which are 1) acetoacetic acid (AcAc), 2) β-hydroxybutyric acid (3-OHBA), and 3) acetone. Concentration increases and decreases alternately between AcAc and 3-OHBA, which has biological effect as ketone bodies [16,17].
On the other hand, from the clinical point of view, hyperketonemia has been usually classified into diabetic ketoacidosis (DKA) and physiological ketosis. The former is observed in extremely elevated blood sugar with acidosis. The latter is observed in normal blood sugar or during a prolong fast without clinically risky acidosis [18], and is from persisting starvation or ketogenic diet (KD). A ketogenic diet (KD) has traditionally comprised high fat, moderate/ low protein, and very low carbohydrate intake and aimed to induce a state of nutritional ketosis [19].
In the category of LCD by Feinman and Bernstein, it is called Very Low-Carbohydrate Ketogenic Diet (VLCKD). The characteristic points of VLCKD are in the following. It contains of carbohydrate about 20-50 g/d or <10% of the 2000 kcal/d diet, whether or not ketosis occurs, and derived from levels of carbohydrate required to induce ketosis in most people, with recommendation for early phase of popular diets such as Atkins Diet or Protein Power [7]. Consequently, hyperketonemia has been recognized to be clinically stable and safe condition as the secondary effect of VLCKD.
We have treated many patients with diabetes and metabolic syndrome by clinically application of LCD for years. In this study, we investigated the patient with type 2 diabetes mellitus (T2DM), who started super LCD meal describing the detail analysis of carbohydrate intake for long time, associated with remarkable elevated serum ketone bodies.
Case Presentation
The patient was 61 year-old female, who has been teaching yoga for years. When she was 51 years old, she was pointed out as T2DM. During treatment of oral agents, her liver function tests developed abnormality. Then, she discontinued the therapy, and she herself continued just meal and exercise therapy for 10 years.
She occasionally attended our medical seminar for LCD, then she came to check diabetic status. The HbA1c level was 10.5%, and she visited our diabetic clinic 2 weeks later. Consequently, we started further evaluation and treatment for diabetes.
In first contact, she showed no particular symptoms such as thirsty, polydipsia, polyuria, fatigue or weight loss which are characteristic for diabetes. On physical examination, she showed 158 cm in height, 53 kg in weight, BMI 21.2 kg/m2. Her vitals and consciousness are normal, and lung, heart, abdomen and neurological findings were unremarkable.
Laboratory tests
General laboratory data were as follows: Hb 15.2 g/dl, WBC 4400/μL, Alb 5.0 g/dL, Triglyceride 43 mg/dL, HDL-C 89 mg/dL, LDL-C 152 mg/dL. There were no abnormal results in serum amylase, TSH, free T4, liver function tests.
Specific laboratory data concerning diabetes were as follows: HbA1c 9.4%, blood glucose 178 mg/dL, Immunoreactivity insulin (IRI) 2.9 μU/mL (3-15), HOMA-R 1.28, HOMA-β 9.01, serum C-peptide reactivity (s-CPR) 1.0 ng/mL (1.14.4), urinary C-peptide reactivity (u-CPR) 15 mg/day (28-120), Total ketone bodies 3081 μmol/L (28120), acetoacetic acid (AcAc) 300 μmol/L (1468), 3-hydroxybutyric acid (3-OHBA) 2781 μmol/L (074), Autoantibodies to Glutamate decarboxylase (GADA) <1.4 U/ml (<1.4), Islet cell autoantibodies (IA-2) <0.4 U/ml (<0.4). Glucagon test revealed that s-CPR increased from 1.0 to 1.8 ng/mL in response to glucagon injection. Chest X-P and abdominal CT scan revealed unremarkable findings.
Diet therapy for super LCD
As to the diet therapy for diabetes, the options were proposed for the patient to choose whether traditional calorie restriction (CR) diet or low carbohydrate diet (LCD). She chose LCD with her perfect understanding for the medical knowledge as a yoga teacher.
Furthermore, we proposed 3 kinds of LCD, which are super LCD with 12% of carbohydrate, standard LCD with 26% of carbohydrate and petit LCD with 40% of carbohydrate. We consulted the detail of actual LCD continuation, and decided to choose super LCD.
The detail of the LCD was calculated as follows: ideal weight (kg) is 1.58 × 1.58 × 22=54.9 kg, daily calorie taken per day is 54.9 kg × 25 kcal/kg/day=1373 kcal/day, which is approximately 1400 kcal/day.
We adopted super-LCD formula meal with 12% of carbohydrate which was originated by Dr. Ebe, one of the authors [8-11]. Consequently, the calculation was that 1400 kcal × 0.12=168 kcal by carbohydrate per day, and 168 kcal/4 kcal=42 g of carbohydrate in a day.
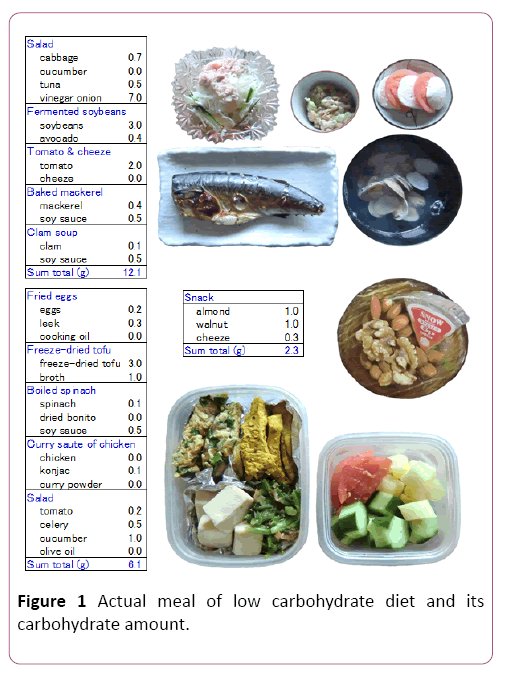
Patient could make the menu of LCD and also cook with less carbohydrate. Some samples from the actual meals are shown in Figure 1, in which perfect calculation of each food including carbohydrate was found. Generally speaking, Japanese style meal usually contains rice, cereal or noodles. However, the actual meal (Figure 1) has almost none carbohydrate or staple food usually included in Asian countries.
Efficacy of LCD for diabetes
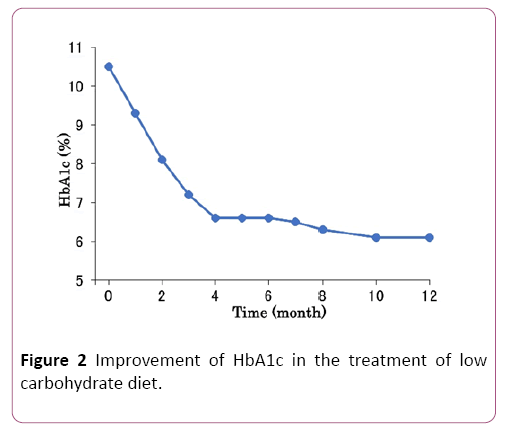
As the patient has started and continued LCD, HbA1c value has decreased from 10.5%, to 9.3% 8.1%, 7.2% and 6.6% in 4 months (Figure 2). After that, HbA1c maintained stable in normal range from 4 to 12 months (Figure 2).
Blood glucose levels were around 170 mg/dL in 0-3 months, 150 mg/dL in 4-7 months and 130 mg/dL in 8-12 months. The values of IRI were stable from 2.9 μU/mL to 4.8 μU/mL during 12 months. The values of serum CPR were stable from 0.9 ng/mL to 1.3 ng/mL during 12 months.
Correlations of biomarkers
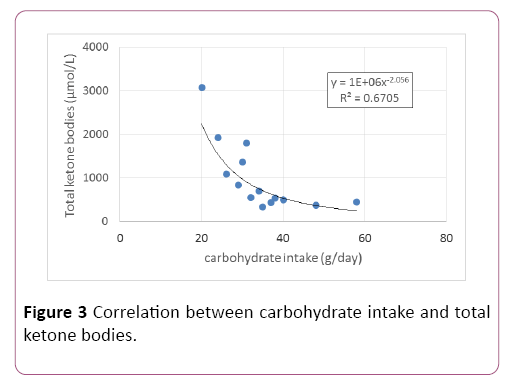
The patient has continued LCD, and showed the elevated blood ketone bodies. She also continued taking food photograph and carbohydrate analyses every day. Consequently, the precise relationship between carbohydrate intake amount and the serum level of ketone bodies during 12 months could be investigated, which indicated the significant correlation between the both factors (p<0.05) (Figure 3). When the carbohydrate amount is about less than 30 g/day, total ketone bodies (T-KB) was increased to moderate to high extent. When the carbohydrate amount is 40-60 g/day, T-KB was increased to moderate extent.
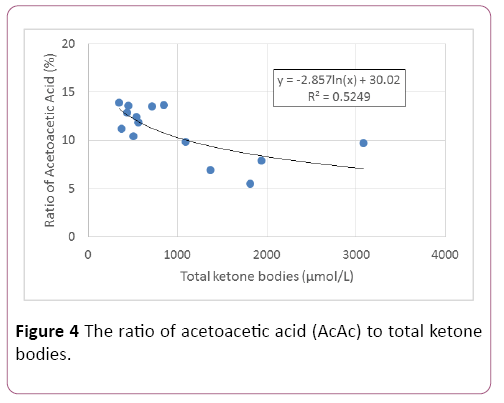
In clinical laboratory examination, total ketone bodies (T-KB) includes 2 fractions, which are acetoacetic acid (AcAc) and 3- hydroxybutyric acid (3-OHBA). The ratio of AcAc/T-KB was investigated, which showed the significant correlation with TKB level (p<0.05) (Figure 4). When the T-KB is less than 1000 μmol/L, AcAc ratio revealed approximately 15 -20%. When the T-KB is more than 1000 μmol/L, AcAc ratio revealed around 10% (Figure 4).
For statistical analyses in this study, correlation coefficients were calculated using Spearman or Pearson test of the Microsoft Excel analytical tool, in reference to the Four steps Excel Statistics 4th edition [20]. A significance level of less than 5% was judged to be statistically significant.
Discussion
The features of this research are summarized as follows: 1) diabetic patient was treated by LCD leading to improved HbA1c, 2) actual carbohydrate amount per day was investigated, 3) significant correlation was shown between carbohydrate amount and serum ketone bodies and 4) ratio of fraction of ketone bodies was examined.
As nutritional therapy, there have been CR and LCD so far. Standard CR diet in Japan was decided according to the guideline of Japan Diabetes Society, in which PFC ratio is 14.7%, 26.9%, 58.4%, respectively [21]. This ratio has not been changed from 1985 to 2015 on the national survey [22]. In general, PFC ratio has been approximately 15:25:60.
On the other hand, authors proposed three patterns of LCD, which are super LCD, standard LCD and petit LCD. The carbohydrate ratio of them are, 12%, 26% and 40%, respectively. Thus, super LCD has nutritional balance with carbohydrate 12%, protein 32% and fat 56% [8-11].
In United States, American Diabetes Association (ADA) recommended that carbohydrate intake per day would be less than 130 g or less than 26% total energy per day [23,24]. This ratio of 26% is consistent with the standard LCD among the three types of LCD that we have proposed so far.
The definition of LCD has been waited worldwide, because there are lots of nutritional pattern and food habits. Along with the definition of Bernstein et al., nutrition diet has been classified into several categories [7]. They are 1) Very lowcarbohydrate ketogenic diet (VLCKD): Carbohydrate, 20–50 g/d or <10% of the 2000 kcal/d diet, 2) Low-carbohydrate diet: <130 g/d or <26% total energy, 3) Moderate-Carbohydrate Diet: 26%–45%, 4) High-Carbohydrate Diet: >45%-201) [7].
Super-LCD is one of VLCKD, and contains 12% of carbohydrate. Continuing VLCKD makes the patient elevated ketone bodies and weight reduction due to ketogenesis [25-28]. With this effect of LCD, authors have treated patients and developed LCD for years [10,11,13,29].
In this study, super LCD formula meal was continued, associated with elevated ketone bodies in blood. The theoretical standard of carbohydrate intake was 42 g per day, according to the calculation of body size. In fact, the patient herself devised a meal and checked the detail amount of carbohydrate every day. Actually, the patient had carbohydrate 7 to 24 g per serving, about 20 to 40 g/day per day, when carbohydrate restriction began.
Such actual detail report would be rather rare and highly evaluated in clinical practice. These limitations gradually relaxed according to the clinical course, associated with decreasing of HbA1c. There was a significant correlation between carbohydrate intake amount and ketone body concentration, which would be remarkable meaningful data.
Concerning the treatment with LCD, ketogenic diet has been involved in the important role. Under normal physiological conditions, cells acquire energy from glucose in the process of glycolysis. As carbohydrate intake is remarkably limited, glycogen stores in the liver and skeletal muscles would be decreased [30,31]. Our body responds by shifting part of the energy source to adipose tissue and utilizing ketone bodies as by-products. Therefore, ketosis is a metabolic state that generates energy from these ketone bodies. The rate that body can supply fuel to the brain and the body is usually 0.5 to 3.0 mg/dL.
Recent studies found that Ketogenic diet would indicate beneficial effect during aerobic performance and significant improvements in maximal oxygen uptake (V̇O2max) and lactate threshold [32]. There are a significant reduction in the time for 2,000 m sprint cycle and in aerobic fatigue [33]. Furthermore, ketogenic diet showed 2-fold increase in peak fat oxidation and 59% increase in mean fat oxidation during submaximal exercise [34]. Furthermore, increased fat oxidation would induce lower respiratory exchange ratio (RER), and improve physical fitness variables such as V̇O2max, lactate threshold, and maximum heart rate [35].
When lipids burn in the body, blood ketone bodies are produced. From the biochemical point of view, ketone bodies include three elements, which are AcAc, 3-OHBA and acetone. Concentration increases and decreases alternately between AcAc and 3-OHBA, and acetone has no biological effect. The degree of fat burning is estimated by measuring AcAc and 3- OHBA. If it is high, it has the evidence that fat is burning at present. In clinical practice, AcAc and 3-OHBA are summed up and measured as total ketone bodies.
In this study, the ratio of AcAc and 3-OHBA in total ketone bodies were investigated. There is two pathophysiological case in hyperketonemia, which are diabetic ketoacidosis (DKA) and physiological ketosis. DKA revealed that blood glucose level is more than 300 mg/dL associated with acidosis, and ketone bodies level would be about 20-25 mmol/L (20,000-25,000 μmol/L) [18,36]. Previous report concerning DKA revealed that the average data were glucose 650 mg/dL, pH 7.13, T-KB 10.2 ± 1.8 mmol/L, AcAc 2.7 ± 0.5 mmol/L, 3-OHBA 7.5 ± 1.3 mmol/L and the ratio of 3-OHBA 74% [37].
On contrast, in physiological ketosis, blood glucose is normal and plasma ketone bodies would increase to 6-8 mmol/L (6000-8000 μmol/L) during a prolonged fast [18]. The cause would be from prolonged starvation and ketogenic diet, which was proposed by biochemist Crebs given Nobel Prize [38].
In recent years, clinical significance of hyperketonemia has been in focus, because of the possibilities for various beneficial function [39-41]. Regarding the fragments of ketone bodies, 3- OHBA has been said to express the various efficacy and has acted as a ligend to the G-protein coupled GPR 109, resulting in anti-inflammatory properties [15,41,42]. Consequently, current results concerning the ratio of AcAc and 3-OHBA would be the fundamental data for future research.
The beneficial function of ketone bodies will be more in focus in anti-aging medicine. Several clinical positive effects are as follows: Ketone bodies can burn fatty acids well, becomes healthy and excellent diet, suppresses aging caused by hyperglycemia, develops to comprehensive anti-aging, and prevents dementia. In this way, by limiting carbohydrate intake, the switch in the ketone body circuit becomes turning on.
As a result, the longevity gene Sirt 3 is activated, and the metabolism of the ketone body is further promoted. Furthermore, continuation of exercise increases the expression of Sirt 3 in the human body, and Sirt 3 increases intramuscularly [43,44]. Thus, carbohydrate restriction plus exercise leads humans to the health and longevity path.
We have discussed concerning LCD and hyperketonemia. Regarding the future directions and recommendations for clinical research and treatment, we can speculate as follows [15,39-41,45]: 1) There are too many patients with diabetes worldwide associated with diabetic macrovascular and microvascular complications, 2) Rapid normalization of profile of blood glucose would be necessary in order to prevent arteriosclerotic influence with diabetes, 3) For their nutritional therapy, LCD than CR would be rather recommended for its beneficial efficacy, 4) It has two benefits, which are rapid lowering effects of blood glucose and persisting elevated ketone bodies, 5) hyperketonemia would reduce the risk of metabolic / cardiovascular / renal / neural systems, antiarteriosclerotic effect, anti-cancer action, and so on. Consequently, obtained data in this study would be a useful reference for further development of clinical research and treatment.
Conclusion
Current study revealed that the case treated with super LCD containing 12% carbohydrate showed detail carbohydrate intake records for years, remarkable decrease of HbA1c value, significant correlation between carbohydrate intake and serum ketone bodies. In elevated ketone bodies, the ratio of AcAc and 3-OHBA in total ketone bodies were investigated. These results would become the fundamental data and suppose future directions and recommendations for research of ketone bodies in low carbohydrate diet.
Acknowledgement
The authors would like to thank the patients and staffs for their cooperation and support. The authors declare that they have no conflicts of interest.
References
- Atkins R (1998) Dr. Atkins’ new diet revolution.Avon books, New York.
- Bernstein RK (2007) Dr. Bernstein’s Diabetes solution: The complete guide to achieving normal blood sugars. Little, Brown US, New York.
- Shai I, Schwarzfuchs D, Henkin Y (2008) Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 359: 229-241.
- Schwarzfuchs D, Golan R, Shai I (2012) Four-year follow-up after two-year dietary interventions. N Engl J Med 367: 1373-1374.
- Meng Y, Bai H, Wang S, Li Z, Wang Q (2017) Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: A systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract 131:124-131.
- Namazi N, Larijani B, Azadbakht L (2017) Low-carbohydrate-diet score and its association with the risk of diabetes: A systematic review and meta-analysis of cohort studies. Horm Metab Res 49:565-571.
- Feinman RD, Pogozelski WK, Astrup A, Bernstein RK, Fine EJ, et al. (2015) Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition 31:1-13.
- Ebe K, Ebe Y, Yokota S (2004) Low Carbohydrate diet (LCD) treated for three cases as diabetic diet therapy. Kyoto Med Association J 51: 125-129.
- Bando H, Nakamura T (2008) Carbo-count therapy and low carbohydrate diet (LCD). The J Therapy 90: 3105-3111.
- Bando H, Ebe K, Muneta T, Bando M, Yonei Y (2017) Clinical effect of low carbohydrate diet (LCD): Case report. Diabetes Case Rep 2: 124.
- Ebe K, Bando H, Yamamoto K, Bando M, Yonei Y (2018) Daily carbohydrate intake correlates with HbA1c in low carbohydrate diet (LCD). J Diabetol 1: 4-9.
- Muneta T, Kawaguchi E, Nagai Y, Matsumoto M, Ebe K (2016) Ketone body elevation in placenta, umbilical cord, newborn and mother in normal delivery. Glycative Stress Research 3: 133-140.
- Ebe K, Bando H, Muneta T, Bando M, Yonei Y (2017) Effect of low carbohydrate diet (LCD) for diabetic patients with hypertriglycemia. Endocrinol Metab 1: 104.
- Cahill GF (1970) Starvation in man. N Engl J Med 282:668-75.
- Watanabe S (2016) Wellness fasting and hyperketosis. Diabetes Res Open J 2: e10-e13.
- Laffel L (1999) Ketone bodies: A review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev 15: 412-426.
- Cahill GF (2006) Fuel metabolism in starvation. Annu Rev Nutr 26:1-22.
- Paoli A (2014) Ketogenicdiet for obesity: Friend or foe? Int J Environ Res Public Health 11: 2092-2107.
- Freeman JM, Kossoff EH, Hartman AL (2007) Theketogenic diet: One decade later. Pediatrics 119: 535-543.
- Yanai H (2015) Four step excel statistics (4th edn.).Seiun-sha Publishing Co.Ltd, Tokyo.
- Japan Diabetes Association (2013) Diabetes clinical practice guidelines based on scientific evidence.
- The Ministry of Health and Welfare, Japan (2015) National Health Nutrition Survey Result.
- American Diabetes Association (2013) Nutrition recommendations and interventions for diabetes. Diabetes Care 36:S12-32.
- International Diabetes Federation (2015) Standards of medical care in diabetes-2015. Diabetes Care 38: S1-S94.
- Saslow LR, Kim S, Daubenmier JJ, Moskowitz JT, Phinney SD, et al. (2014) A randomized pilot trial of a moderate carbohydrate diet compared to a very low carbohydrate diet in overweight or obese individuals with type 2 diabetes mellitus or prediabetes. PLoS ONE 9: e91027.
- Hussain TA, Mathew TC, Dashti AA, Asfar S, Al-Zaid N (2012) Effect of low-calorie versus low-carbohydrate ketogenic diet in type 2 diabetes. Nutrition 28:1016-1021.
- Watanabe S, Hirakawa A, Utada I, Aoe S, Moriyama S, et al. (2017) Ketone body production and excretion during wellness fasting. Diabetes Res Open J 3: 1-8.
- Snorgaard O, Poulsen GM, Andersen HK, Astrup A (2017) Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care 5:e000354.
- Bando H, Ebe K, Muneta T, Bando M, Yonei Y (2017) Effect of low carbohydrate diet on type 2 diabetic patients and usefulness of M-value. Diabetes Res Open J 3: 9-16.
- Nilsson LH, Furst P, Hultman E (1973) Carbohydrate metabolism of the liver in normal man under varying dietary conditions. Scand J Clin Lab Invest 32: 331-337.
- Phinney SD, Bistrian BR, Evans WJ, Gervino E, Blackburn GL (1983) The human metabolic response to chronic ketosis without caloric restriction: Preservation of submaximal exercise capability with reduced carbohydrate oxidation. Metabolism 32: 769-776.
- Zajac A, Poprzecki S, Maszczyk A, Czuba M, Michalczyk M, et al. (2014) The effects of a ketogenic diet on exercise metabolism and physical performance in off-road cyclists. Nutrients 6: 2493-2508.
- Rhyu HS, Cho SY (2014) The effect of weight loss by ketogenic diet on the body composition, performance-related physical fitness factors and cytokines of taekwondo athletes. J Exerc Rehabil 10: 326–331.
- Volek JS, Freidenreich DJ, Saenz C, Kunces LJ, Creighton BC, et al. (2016) Metabolic characteristics of keto-adapted ultraendurance runners. Metabolism 65: 100-110.
- Ramos-Jimenez A, Hernandez-Torres RP, Torres-Duran PV, Romero-Gonzalez J, Mascher D, et al. (2008) The respiratory exchange ratio is associated with fitness indicators both in trained and untrained men: A possible application for people with reduced exercise tolerance. ClinMed CircRespiratPulm Med 2: 1-9.
- Paoli A, Rubini A, Volek JS, Grimaldi KA (2013) Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J ClinNutr 67: 789-796.
- Matsumoto H (1992) Pathophysiological studies on 59 patients with diabetic ketoacidosis and immunohistological examination on pancreatic islets. J Tokyo Wom Med Univ 62:1598-1607.
- Krebs HA (1966) The regulation of the release of ketone bodies by the liver. Adv Enzyme Regul 4: 339-354.
- Veech RL (2004) The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: Ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. Prostaglandins Leukot Essent Fatty Acids 70: 309-319.
- Kossoff EH, Zupec-Kanici BA, Amask PE (2009) Optimal clinical management of children receiving the ketogenic diet: Recommendations of the International Ketogenic Diet Study Group. Epilepsia 50: 304-317.
- Shimazu T, Hirschey MD, Newman J (2013) Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science 339: 211-214.
- Youm YH, Nguyen KY, Grant RW, Goldberg EL, Bodogai M, et al. (2015) Ketone body β-hydroxybutyrate blocks the NLRP3 inflammasome-mediated inflammatory disease. Nat Med 21: 263–269.
- Newman JC, Verdin E (2014) Ketone bodies as signaling metabolites. Trends Endocrinol Metab 25: 42–52.
- Edwards C, Copes N, Bradshaw PC (2015) D-ß-hydroxybutyrate: an anti-aging ketone body. Oncotarget 6: 3477–3478.
- Kavalek M, Gannon R, Nelson M (2017) A case for and against ketogenic diets in athletes. Strength and Conditioning Journal 39: 27–31.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences