Ionizing Radiation Side Effects on Salivary Glands Post External Beam Radiation Therapy of Head and Neck Tumors
Mpumelelo Nyathi*
Department of Medical Physics. School of Medicine, Sefako Makgatho Health Sciences University, Ga-Rankuwa, South Africa
- *Corresponding Author:
- Mpumelelo Nyathi
Department of Medical Physics. School of Medicine
Sefako Makgatho Health Sciences University, Ga-Rankuwa, South Africa.
Tel: +0027780203216
E-mail: mpumelelo.nyathi@smu.ac.za
Received Date: November 11, 2017; Accepted Date: February 03, 2018; Published Date: February 25, 2018
Citation: Nyathi M (2018) Ionizing Radiation Side Effects on Salivary Glands Post External Beam Radiation Therapy of Head and Neck Tumors. J Biol Med Res. Vol.2 No.1:4
Abstract
Introduction: External beam radiation therapy is a treatment modality for a group of malignancies clustered under one diagnostic heading as head and neck tumors. These tumors can be found in the oral cavity, larynx, nasopharynx, hypopharynx, nose, cervical esophagus, nose, lips and paranasal sinuses. The external beam radiation therapy relies on ionizing radiation to destroy the deoxyribonucleic acid (DNA) of the malignant cells leading to their death. This study aimed at examining the side effects of ionizing radiation on salivary glands post radiation therapy of head and neck tumors.
Methods: A literature search using Google search engine, Science Direct and Medline was conducted to find publications detailing the side effects of ionizing radiation on the salivary glands and the consequential effects on the quality of life of people previously treated for head and neck tumors using external radiation beam therapy.
Results: Ionizing radiation causes structural and physiological alteration of the salivary glands resulting in reduced functional capacity and reduced saliva flow rates. People previously treated for head and neck tumors suffer from dry mouth, dental caries, oral candidiasis, mouth pain and sleeping problems.
Conclusion: People treated for head and neck tumors with ionizing radiation suffer from dry mouth, dental caries, and malnutrition among other associated health problems.
Keywords
Salivary glands; External beam radiation therapy; Dry mouth; Ionizing radiation
Introduction
External beam radiation therapy is a treatment modality for a group of malignancies clustered under one diagnostic heading as head and neck tumors [1]. Radiation therapy may be administered post-surgery. However, depending on the nature of the tumors, these tumors may be treated using the external beam without surgery. Furthermore, external radiation beam therapy may also be used in combination with chemotherapy [2]. However, it has since been established that the external beam radiation therapy technique leads to salivary gland injury resulting in long term health complications for people previously treated for head and neck tumors [1-3].
Literature Review
Treatment of head and neck tumors with external radiation beam may involve use of any of the following techniques; intensity-modulated radiation therapy (IMRT), two-dimensional radiation therapy (2D-RT) and three-dimensional conformal radiation therapy (3D-CRT) [4]. The external beam radiation therapy relies on the use of ionizing radiation to destroy the DNA of the malignant cells leading to their death [1]. Treatment may last between three and seven weeks. However, this depends on tumor size and the purpose of treatment whether it is curative or palliative. The head and neck tumors maybe treated with doses of between 50 Gy and 70 Gy. A patient would generally receive 2 Gy a day in a week of five consecutive days excluding weekends [2].
The IMRT is the most favorable technique during radiation therapy of head and necks tumors because it has the potential to spare the parotid glands from the intense radiation beam [4] thus reducing the impact of the long-term complications among which may include; xerostomia, hoarseness and erythema [3]. However, radiation treatment despite its effectiveness on tumor destruction leads to side effects that contribute to a low quality of life for people previously treated for head and neck tumors [5].
The head and neck tumors occur in various anatomical parts of the head and neck which include; the oral cavity, the larynx, the nasopharynx, the hypopharynx, the nose, the cervical esophagus, the lips and the paranasal sinuses [1]. The most common type of head neck tumors is the squamous cell carcinoma. The highest incidences of head and neck cancers are the lip and oral cavity cancers and the thyroid cancers. The salivary glands tumors, sarcomas and lymphomas constitute another group of head and neck carcinoma [2].
The salivary glands can be categorized into major and minor [1]. The major salivary glands are the paired parotid, submandibular and the sublingual [1,4]. The minor salivary glands vary from one individual to the other and they are found on their lips, in the inner cheek area or throughout the pharynx [6,7].
Salivary glands consist of many functional units called the acini which encompasses of the myoepithelial cells, connective tissue and the collecting ducts [1,8,9]. The acinar cells can either be mucous or serous in nature [8,9]. The secretions (saliva) produced by the acini are fluid in nature. They comprise of water, enzymes, electrolytes and mucus [6]. The secretions pass through a series of intercalated ducts, past striated ducts and terminal lobular ducts until they reach the main ducts which transport them to the oral cavity [10].
The salivary glands and the ducts cells are often referred to as “reverting post mitotic cells”. Regeneration is through proliferation of secretory and duct cells. The acini are replenished by stem cells in the distal segments of the duct system [10]. The saliva secreted by the acini apparatus is controlled by the autonomic nervous system. Most of it is produced by the parotid, submandibular and sublingual glands [6,8]. The parotid salivary glands produce most of the saliva either when eating or under stimulation while the submandibular salivary glands are responsible for production of most of the saliva while at rest [4].
The minor salivary glands produce a small quantity of saliva [6,8]. However, most of the mucins are produced by the minor salivary glands and the submandibular glands. The mucins are responsible for oral lubrication while also conferring a sense of hydration thorough absorption of water molecules as well as adhering to the mucosa [4]. This study aimed at examining the side effects of ionizing radiation on salivary glands post external beam radiation therapy of head and neck tumors.
Materials and Methods
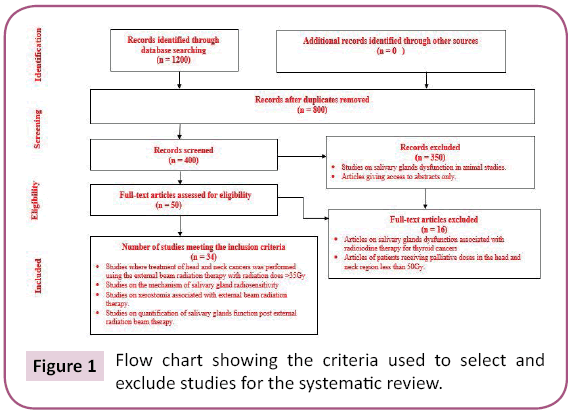
A systematic literature review using Google search engine, Sciencedirect.com and Medline was conducted for publications on salivary gland anatomy, radio sensitivity, injuries following treatment of head and neck tumors using radiation therapy. Abstracts and full texts were thoroughly examined to extract information related to salivary glands anatomy, external radiation beam treatment techniques, side effects associated with treatment and lastly the quality of life of people post treatment for head and neck tumors. Only articles written in English were considered. Additional information was obtained from the articles listed in the references of the articles obtained using the search engines. Articles that presented information of salivary glands injury following radioiodine treatment of thyroid cancers were excluded even though they had information related to salivary glands injury because of radiation injury.
An initial search yielded over 1200 articles. However, these narrowed to 34 after restricting the treatment technique to external beam radiation therapy (Figure 1).
Results
From most of the articles meeting the selection criteria (Table 1), it was established that people treated for head and neck cancers may develop oral cavity complications [1-5,11-13]. Atri et al. [14] established that irradiated serous acinar cells of the parotid and the submandibular salivary glands undergo interphase death. A closer analysis of Table 1 shows that xerostomia is the most common oral complication. As many as 73.5 to 93% of people previously treated for head and neck showed symptoms of xerostomia. Those with severe xerostomia were found to exhibit diminished abilities of chewing and swallowing food, often leading to malnutrition and weight loss. In cases where patients experienced insufficient saliva flow rates results, in formation of dental curies, wearing of dentures, mouth pain, and oral infections, tasting disorders and sleeping problems [15-19]. It was also established that patients may awake at night with the tongue adhered to the hard palate and may have to manually remove the thick saliva.
| Author/ journal/year | Reference | Study design | Sample size | Results |
|---|---|---|---|---|
| Pinna et. al. (2015) Xerostomia induced by radiotherapy: an overview of the physiopathology, clinical evidence, and management of the oral damage. TherClin Risk Manag 11: 171-188. | 12 | Systematic literature Review | 70 articles | Ionizing radiation damages the salivary glands tissue. |
| Severe tissue damage at doses greater than 52Gy. | ||||
| Reduction of saliva output due to damage of salivary tissue is observed at onset of treatment up to 3 months after therapy | ||||
| Treatment results in alteration of saliva electrolyte levels; sodium chloride, calcium and magnesium levels increase whereas potassium is minimally affected. | ||||
| Secreted saliva post radiation found to be vicious with reduced pH in the range 5.0 to 7.0; may turn yellow, brown or even white. | ||||
| Lack of saliva because of salivary glands injury may result in angular cheilitis, cracked lips, periodontal disease, aching of the mouth and halitosis. | ||||
| Lack of saliva may also lead to loss of appetite as the dry mouth makes eating and swallowing difficult. | ||||
| Patients treated for head and neck tumours may lose sense of taste. | ||||
| Konings et al. (2004) On the Mechanism of salivary gland sensitivity. Int J Radiat Oncol Biol Phys 62: 1187–1194. | 13 | Systematic review of literature | 71 articles | Irradiation of salivary glands leads to the leakage of granules and subsequent lysis of acinar cells. |
| Mechanism of damage of both the parotid and submandibular glands is alike despite them having different cell composition. | ||||
| The water secretion is hampered during the first days after irradiation using a single dose. | ||||
| Gómez GJA et al. (2017) Alterations found in the mouth of patients treated with head and neck radiotherapy. Medellin, Colombia. RevistaOdontológica Mexicana 86-96. | 14 | Exploratory Study | 52 patients | High frequency of oral alterations in patients subjected to external beam radiation dosage varying from 3001 to 5 000 cGy |
| Hyposalivation common in patients with stage IV tumours (50%). | ||||
| Hawkins et al. (2018) Sparing all salivary glands with IMRT for head and neck cancer: Longitudinal study of patient-reported xerostomia and head-and-neck quality of life. Radiother Oncol 126: 68-74. | 15 | Longitudinal institutional review | 252 patients | Damage to the parotid salivary glands is dose related. |
| Xerostomia associated with irradiation of salivary glands is dose dependent. | ||||
| Reduction of dose minimises salivary gland damage and reduces xerostomia. | ||||
| So WKW et al. (2012) Quality-of-life among head and neck cancer survivors at one year after treatment – A systematic review. Eur J Cancer 48: 2391-2408. | 16 | Systematic literature review | 37 studies | Irradiation of salivary glands resulted in secretion of sticky saliva. |
| Deterioration of the functioning of salivary glands | ||||
| Maes et al (2002) Preservation of parotid function with uncomplicated conformal radiotherapy. Radiother Oncol 63: 203-211. | 17 | Prospective cohort study | 39 patients | The parotid salivary should at least receive <20Gy to spare them from severe radiation injury that leads xerostomia. |
| Verdonck-de Leeuw et al. (2008) Impact of Late Treatment-Related Toxicity on Quality of Life Among Patients with Head and Neck Cancer Treated with Radiotherapy. J Clin Oncol 26: 3770-3776. | 18 | Prospective cohort study, assessments of patients taking place at 6,12,18, and 24 months after completion of radiotherapy | 425 disease free patients | Radiation induced xerostomia found to be the most advert side effect of radiation therapy of head and neck tumours arising from irradiation of salivary glands. |
| Patients treated for head and neck tumours registered swallowing problems | ||||
| Kakoei et al. (2012) Xerostomia after Radiotherapy and its Effect on Quality of Life in Head and Neck Cancer Patients. Arch Iran Med 15: 214-218. | 19 | Longitudinal prospective study of 63 patients assessed over six months, the subjects were selected from the only radiotherapy referral center at Shafa Hospital, Kerman, Iran | 63 patients | The quantity of saliva did not change significantly during therapy |
| Patients suffered xerostomia after treatment due to permanent damage of salivary glands in the treatment zone. | ||||
| Chambers et al. (2004) Radiation-induced xerostomia in patients with head and neck cancer: pathogenesis, impact on quality of life, and management. Head Neck 26: 796-807. | 20 | Systematic literature review | 73 articles | Xerostomia causes oral discomfort and pain, increased dental caries, oral infection, difficulty speaking and swallowing. |
| Xerostomia significantly impairs the quality of life of patients treated for head and neck malignancies and can compromise nutritional intake and continuity of cancer therapy. | ||||
| Acute xerostomia results in oral mucositis, infection, fungal, bacterial, sialadenitis and taste dysfunction. | ||||
| Chronic xerostomia leads to soft-tissue necrosis, dental caries. | ||||
| Preethi et al. (2011) Assessment of parotid salivary gland function in head and neck tumours receiving radiation therapy of head and neck cancer patients receiving radiation therapy using quantitative salivary gland scintigraphy. Pak J Physiol 7:1 | 21 | Prospective salivary gland study | 35 patients planned for radiotherapy for head and neck tumours | Severe salivary glands dysfunction for patients receiving radiation doses greater than 50 Gy. |
| The submandibular salivary glands and the sublingual salivary glands are less radiosensitive compared to the parotid salivary glands | ||||
| Atri et al. (2007) Management of Radiation Induced Xerostomia in Head and Neck Cancers. J Oral Health Comm Dent 1: 33-39 | 22 | Systematic literature review | 32 Sample sizes | Dose tolerance of salivary glands varies between 32Gy and 46Gy. |
| Curative external beam radiotherapy is usually 60Gy or more, however results in a complication called xerostomia. | ||||
| Xerostomia, interferes with chewing and nutrition, deterioration of oral hygiene, dental curies, | ||||
| Plemons et al (2015) Managing xerostomia and salivary gland | 23 | Systematic literature review | 80 articles | Xerostomia is the most common symptom of salivary gland injury arising from irradiation of head and neck cancer |
| Hypofunction. American Dental Association. | Xerostomia refers to subjective feeling of a dry mouth, may range from mild oral discomfort to significant oral disease that can compromise patients’ health, dietary intake and quality of life. | |||
| Council on Scientific Affairs | ||||
| Baijal et al. (2012) Radiation Induced Xerostomia. Int J Head Neck Sur 3: 82-86. | 24 | Systematic literature review | 39 articles | Irradiation of salivary glands during radiation treatment of head and neck tumours leads to Xerostomia |
| Xerostomia is a late side effect of radiation therapy of head and neck cancers which manifests as dry mouth, sore throat, altered taste, dental decay, changes in the quality of voice, impaired chewing and difficulties in swallowing, nutritional issues and weight loss | ||||
| Deasy et al. (2010) Radiotherapy – Dose – Volume effects on salivary glands function. Int J Radiation Oncology Biol Phys 76: S58-S63. | 25 | Systematic literature review | 31 articles | Irradiation of salivary glands leads to reduction in salivary gland function, accompanied by poor dental hygiene, oral infections, oral pain, difficulty in chewing and swallowing |
| Eisbruch A (2007) Reducing Xerostomia by IMRT: What may, and what may not be, be achieved. J Clin Oncol 25: 4863-4864. | 26 | Systematic literature review | 17 articles | Salivary glands acinar cells apoptosis is associated with low doses while necrosis occurs at high doses |
| Xerostomia is the side effect of external beam radiation therapy of head and neck cancers. | ||||
| Patients havesubjective feeling of dry mouth | ||||
| diminished salivary output resulting in mastication and deglutition difficulties contributing to nutritional deficiencies, predisposing the patient to mucosal fissures, ulcerations, changing composition of the oral flora, promoting dental caries. | ||||
| Tolentio Ede S et al (2011) Oral adverse effects of head and neck radiotherapy: a literature review and suggestion of a clinical oral care guideline for irradiated patients. Journal of Appl Oral Sci 19: 448-454 | 27 | Systematic literature review on oral sequelae from head and neck radiotherapy | 35 articles | Ionizing radiation damages salivary glands resulting in reduced salivary flow rates and change in the composition of saliva. |
| Injury of salivary glands leads to sensation of dry mouth also called xerostomia | ||||
| Glandular changes in salivary glands may lead to permanent inability to release saliva, however, the glandular changes are dose dependent and volume of gland irradiated | ||||
| Functional impairment of salivary glands leads to impaired oral function, burning sensation, cracked lips, increased susceptibility to dental and oral infections. | ||||
| Radiation changes composition of saliva, increasing its viscosity. |
Table 1: Overview of studies including ionizing radiation side effects on salivary glands post external beam radiation therapy of head and neck tumour.
Discussion
Radiation therapy either as full-dose curative treatment or with the palliative intent has been found to be an ideal therapy for head and neck cancers [1-5]. However, during treatment the salivary glands are always included in the radiation field hence their injury leading to dysfunction [11,20-26]. The parotid salivary glands which consist purely of the serous gland [6-9] are the most sensitive compared to the submandibular glands from a clinical perspective [26]. The radio sensitivity of the parotid salivary glands may be because they contain heavy metal granules. During therapy, the ionizing radiation causes the disruption of the metal granules by means of a metal-catalyzed induction of lipid peroxidation causing release of lytic enzymes into the cell’s cytoplasm, hence autolysis and eventual death of the affected cell. However, even though the parotid salivary glands are more radiosensitive compared to the submandibular glands, the damage response by both pairs of the salivary glands is the same [11].
The ionizing radiation causes the salivary glands to undergo structural degradation [1-5,13]. According to Eisbruch [13] the salivary glands acinar cells apoptosis occurs at low doses while necrosis occurs at high doses. Atri et al. [18] found that dose tolerance of the salivary glands varied between 32 Gy and 46 Gy. However, the curative dose of head and neck tumors may rise to 60 Gy or more. This value is well above the dose tolerance range of the salivary glands. Exceeding the dose tolerance range of the salivary glands may lead to permanent injury and dysfunction of the salivary glands and consequential xerostomia. People treated for head and neck tumors may begin to suffer from xerostomia after the start of treatment of head and neck tumors [15]. Xerostomia is a sensation of dry mouth mainly attributed to reduced saliva flow rates, it varies from one patient to the next. However, recovery of salivary function may be temporary or may be permanent [23]. A study by Hawkins et al. [4] concluded that the degree of xerostomia is dose dependent. Therefore, to preserve the function of the salivary glands of people treated for head and neck tumors, it is important that radiation techniques that minimize the intensity of the radiation field on the salivary glands be used.
Zhang et al. [27] established that adaptive radiotherapy reduces the parotid salivary gland mean radiation dose. However, a previous study by Sood et al. [28] encouraged salivary gland transfer before therapy to preserve them from them from radiation injury.
Several researchers have established that xerostomia owing to irradiation of salivary glands may either be acute or chronic [16,19]. However, irrespective of its degree, xerostomia has a deleterious effect on the life of patients treated for head and neck tumors. Baijal et al. [20] reported that people tread for head and neck may experience sore throat, altered taste, dental decay, changes in the quality of voice, impaired chewing and difficulties in swallowing, nutritional issues and weight loss. A further study by Deasy et al. [21] established that people treated for head and neck tumors are highly likely to have difficulties in chewing and swallowing and sleep disturbances. It has also been established that xerostomia may also manifest inform of dry mouth due to reduced saliva output [21,22]. Reduced saliva in the oral cavity leads to oral discomfort, dietary intake and weight loss thus compromising the patients’ health [19]. De Souza Tolentio et al. [23] reported that a compromised integrity of the oral leaves patients prone to infections by bacteria, yeasts and viruses.
Management of patients treated with external beam radiation therapy needs a multidisciplinary approach that should involve physicians and dentists. Andreas and Griffiths [29] proposed use moistening agents and saliva substitute to alleviate the symptoms of xerostomia. De Souza Tolentio et al. [23] reported on studies that encouraged use of antimicrobial agents for prevention of fungal and bacterial infections. They further encourage discontinued use of dentures. However, where the need of dentures was inevitable, they should be cleaned in a solution of 0.5% of hypochlorite solution for 30 minutes.
Despite the knowledge that the degree of injury of the salivary glands is dose related [4,20] the mechanisms of salivary glands degradation by ionizing radiation remains not well understood. Furthermore, the side effects which are a consequence of xerostomia remain difficult to quantify. An attempt by Maes et al. [2] to quantify severity of the salivary glands hypofunction did not have much objectivity due to the listener and patient influence. However, a recent phantom study by Nyathi [30] provided an objective phantom method for quantifying salivary gland function post radiation therapy of head and neck tumors. However, it still must be tested in human studies.
Conclusion
The use of IMRT technique during treatment of head and neck tumors minimizes salivary gland injury thus reducing the degree xerostomia and related side effects among patients treated for head and neck tumor. Prevalence of xerostomia is dose dependent, therefore reducing the intensity of ionizing radiation beam on the salivary glands will reduce the impact of dry mouth and consequences such as dental caries and malnutrition among other associated health problems. Management of people treated for head and neck tumors needs a multidisciplinary approach involving dentists, doctors and clinicians. The dents should be involved with dental care during and post radiation therapy while clinicians should continue to investigate the means of quantifying the degree of xerostomia. Furthermore, clinicians need to determine the methods of alleviating the symptoms of dry mouth to reduce the discomfort arising from reduced saliva production.
References
- Nyathi M (2015) Quantitative evaluation of the parotid and the salivary glands function post radiation therapy of head and neck tumours. Sefako Makgatho Health Sciences University, South Africa.
- Pinna R, Campus G, Cumbo E, Mura I, Milia E (2015) Xerostomia induced by radiotherapy: an overview of the physiopathology, clinical evidence, and management of the oral damage. Ther Clin Risk Manag 11:171-188.
- Lovelace TL, Fox NF, Sood AJ, Nguyen SA, Day TA (2014)Management of radiotherapy-induced salivary hypofunction and consequent xerostomia in patients with oral or head and neck cancer: meta-analysis and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol 117:595-607.
- Hawkins PG, Lee JY, Mao Y, Li P, Green M, et al. (2018) Sparing all salivary glands with IMRT for head and neck cancer: Longitudinal study of patient-reported xerostomia and head-and-neck quality of life. Radiother Oncol 126: 68-74
- So WK, Chan RJ, Chan DNS, Hughes BG, Chair SY, et al. (2012) Quality-of-life among head and neck cancer survivors at one year after treatment-A systematic review. Eur J Cancer 48:2391-2408.
- Fehrenbach MJ, Herring SW (2007)Illustrated anatomy of the head and neck. St Louis: Saunders Elsevier.
- Tucker AS (2007) Salivary gland development. Sem Cell Biol18:237-244.
- Beale T, Madani G (2006) Anatomy of the salivary glands: Semin Ultrasound CT and MRI 2:436-439.
- Baert AL, Sartor LK (2006) Head and neck cancer imaging. Berlin: Springer-Verlag Heidelberg, Germany.
- Jane LW (1995) Imaging of the salivary glands. Semin Ultrasound CT and MRI116:546-568.
- Konings AWT, Copes RP (2004)On the mechanism of salivary gland sensitivity. Int J Radiation Oncology Biol Phys 62:1187-1194.
- Gómez GJA, Camacho RVL, Torres JEB, Gomez SMB, Álzate DPC, et al. (2017) Alterations found in the mouth of patients treated with head and neck radiotherapy. Medellin, Colombia. RevistaOdontológica Mexicana 21: 86-96.
- Maes A, Weltens C, Flamen P, Lambin P, Bogaerts R, et al. (2002) Preservation of parotid function with uncomplicated conformal radiotherapy. Radiother Oncol63: 203-211.
- Atri R, Dhankhar R, Nair V, Kaushal V (2007) management of radiation induced xerostomia in head and neck cancers. J Oral Health Comm Dent 1: 33-39.
- Kakoei S, Haghdoost AA, Rad M, Nakhaei M, Bahador M, et al. (2012)Xerostomia after radiotherapy and its effect on quality of life in head and neck cancer patients. Arch Iran Med15: 214-218.
- Chambers MS, Garden AS, Kies MS, Martin JW (2004) Radiation-induced xerostomia in patients with head and neck cancer: pathogenesis, impact on quality of life, and management. Head Neck26:796-807.
- Preethi BLG, Ulla I, Bhaskar V, Suresh KP, Naveen T (2011)Assessment of parotid salivary gland function in head and neck tumours receiving radiation therapy of head and neck cancer patients receiving radiation therapy using quantitative salivary gland scintigraphy. Pak J Physiol7:1.
- Verdonck-de Leeuw IM, Aaronson NK, Leemans CR, Slotman BJ, DoornaertP (2008) Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol 26: 3770-3776.
- Plemons JM, Al-Hashimi I, Marek CL (2014) Managing xerostomia and salivary gland hypofunction: executive summary of a report from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 145: 867-873.
- Baijal G, Kar R, Agarwal JP (2012) Radiation induced xerostomia. Int J Head Neck Sur 3:82-86.
- Deasy JO, Moiseeko V, Marks L, Chao KS, Nam J, et al.(2010) Radiotherapy dose-volume effects on salivary gland function. Int J Radiation Oncology Biol Phys 76: S58-S63.
- Eisbruch A (2007) Reducing xerostomia by IMRT: What may, and what may not be, be achieved. J Clin Oncol 25: 4863-4864.
- Tolentino Ede S, Centurion BS, Ferreira LH, Souza AP, Damante JH, et al. (2011) Oral adverse effects of head and neck radiotherapy: Literature review and suggestion of a clinical oral care guideline for irradiated patients. J Appl Oral Sci 19: 448-454.
- Liu CC, Xia R, Guadagnolo A, Cormier JN, Du XL (2011) Risk of xerostomia in association with the receipt of radiation therapy in older patients with head and neck cancer. Am J Ther18:206-215.
- Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, et al. (2008)Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol26:3770-3776.
- Avila JL, Grundmann O, Burd R, Limesand KH (2009)Radiation-induced salivary gland dysfunction results from p53-dependent apoptosis. Int J RadiatOnco Bio Phys73: 523-529.
- Zhang P, Simon A, Rigaud B, Castelli B, Ospina Arongo JD,et al. (2016)Optimal adaptive IMRT strategy to spare the parotid glands in oropharyngeal cancer. Radiother Oncol 120:41-47.
- Sood AJ, Fox NF, O‘Connell BP, Lovelace TL, Nguyen SA, et al. (2014) Salivary gland transfer to prevent radiation-induced xerostomia: A systematic review and meta-analysis. Oral Oncol 50: 77-83.
- Andreas N, Griffiths C (2001) Dental complications of head and neck radiotherapy: part 2 (2001) Aust Dent J46:174-82.
- Nyathi M, Sithole ME (2017) Salivary gland scintigraphy with partial volume effects quantification: A phantom feasibility study. Australas Med J 10: 752-758.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences