Improved Survival with a Standardized Multidisciplinary 3-in-1 Pelvic Damage Control Protocol for Hemodynamically Unstable Pelvic Fracture
Janice Lau*, Chui KH, Ip KC, Lee KB and Wilson Li
Queen Elizabeth Hospital, Hong Kong
- *Corresponding Author:
- Janice Lau
Queen Elizabeth Hospital, Hong Kong
Tel: +852 3506 8888
E-mail: laukay@gmail.com
Received date: November 9, 2016; Accepted date: November 28, 2016; Published date: December 3, 2016
Citation: Janice Lau, Chui KH, Ip KC, et al. Improved Survival with a Standardized Multidisciplinary 3-in-1 Pelvic Damage Control Protocol for Hemodynamically Unstable Pelvic Fracture. J Emerg Trauma Care 2016; 1:1.
Abstract
Introduction: Haemodynamically unstable pelvic fracture carries a high mortality rate of up to 60%. Being one of the trauma centers in Hong Kong, we have been developing and modifying a protocol for unstable pelvic fracture since 1996, with continuous improvement in survival rate. In the most updated 3-in-1 Pelvic Damage Control Protocol, three different sources of bleeding, including bony, venous, and arterial bleeding are tackled by external fixation, retroperitoneal pelvic packing and angio-embolization respectively. They are conducted in sequential order in the same operative session and theatre within the golden hour.
Methods: All patients with haemodynamically unstable pelvic fractures managed in our center from 1st January 1996 to 31st December 2015 were retrospectively reviewed. The overall survival rates during different phases of protocol modification were compared.
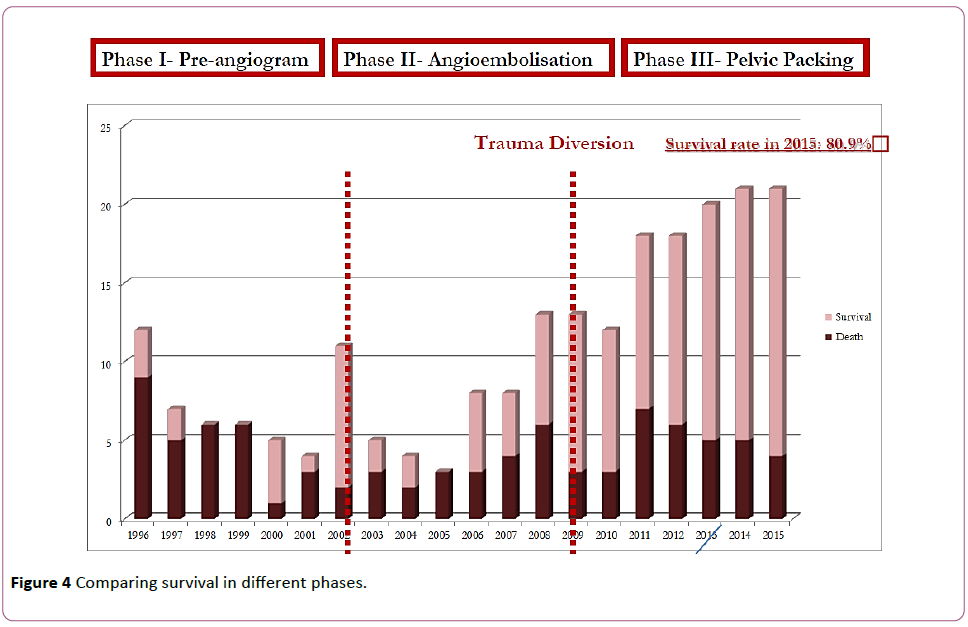
Findings: 210 patients were included. The overall survival had improved from 27% in phase I (1996-2001) with external fixation alone, to 57% in phase II (2002- June 2008) with added angio-embolization, and to 71% in Phase III (July 2008 onwards) with the latest protocol. The survival in phase III has further improved to 81% in 2015. The expected survival of patients also improved as shown in the W-score according to trauma and injury severity score (TRISS).
Conclusion: In hemodynamically unstable pelvic fractures, the use of standardized multidisciplinary protocol results in improved survival. The three different techniques in our protocol are complementary in achieving hemostasis in unstable pelvic fractures.
Keywords
Fracture fixation; Pelvis
Introduction
Hemodynamically unstable pelvic fractures are often associated with high mortalities [1,2]. The management of this group of patient are challenging because they are often involved in high energy trauma with multiple concomitant injuries.
Exsanguinating hemorrhage is the common cause of death in this group of patients. Timely hemostasis is the key to survival. The three sources of bleeding from the broken pelvic ring, namely bony [3], venous [4,5] and arterial [6,7] should ideally all be addressed without delay.
In view of the complexity and difficulties in the management of these patients, establishment of a multidisciplinary protocol is of upmost importance to enhance quality of care, achieve timely hemostasis and thus increase chance of survival [8,9].
In our center, a multidisciplinary protocol has been established since 1996 to guide the management of these patients in the acute setting. Our objective is to evaluate the survival of hemodynamically unstable patients with pelvic fractures.
Materials and Methods
This is a retrospective study from 1st January 1996 to 31st December 2015. All patients with hemodynamically unstable pelvic fractures who were treated in our center were included. The age, sex, injury severity score and data of survival were analyzed.
These patients were all managed according to our local multidisciplinary protocol.
Under the local protocol, hemodynamically unstable patients were defined as those having persistent systolic blood pressure <= 90 mmHg after receiving >= 2000 ml crystalloid intravenously as resuscitation.
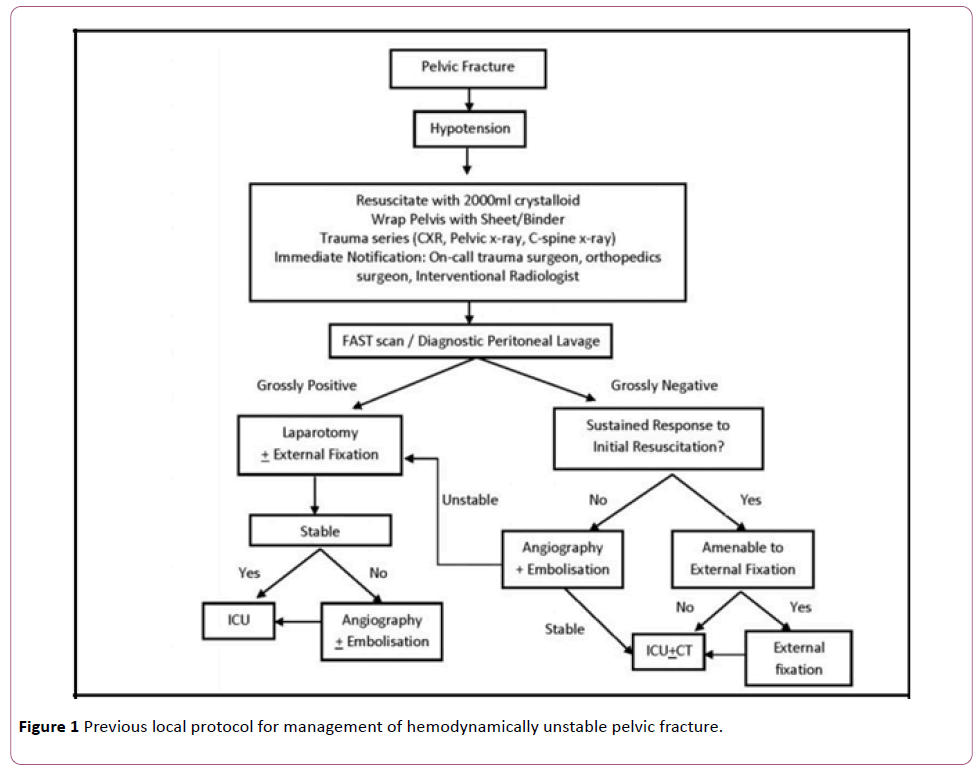
In earlier years, from 1996 till 2001 (Phase I), interventional radiology techniques were not that readily available. During that period, hemodynamically unstable patients with pelvic fractures were managed mainly with resuscitation and pelvic external fixation.
From 2002 onwards, on table angio-embolization had become increasingly assessable, and thus became another important technique for hemostasis. From 2002 to June 2008 (Phase II), under local protocol, patients underwent external fixation if the patients respond to initial resuscitation and the fracture patterns were amendable to such. Angio-embolization was employed when the patients did not have sustained response to initial resuscitation, the fracture patterns were not amendable to external fixation or if the patients remained unstable after external fixation.
Laparotomies were carried out by general surgeons if patients remained unstable after angio-embolization or when there was evidence of intra-abdominal hemorrhage causing the instability Figure 1.
Figure 1: Previous local protocol for management of hemodynamically unstable pelvic fracture.
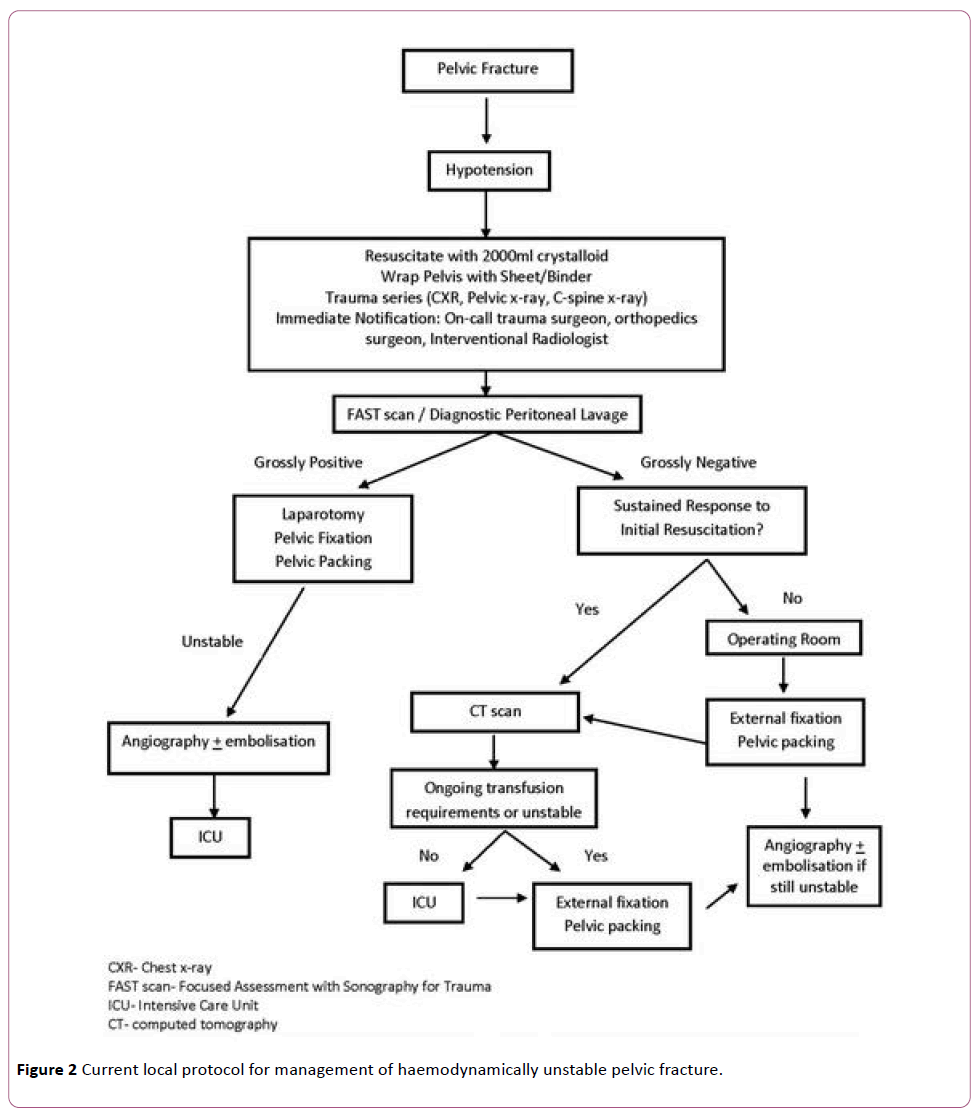
The protocol was modified in 2008 and was used until today (Phase III) with continuous fine-tuning and evaluation. Under the latest protocol, once the patients meet the criteria of hemodynamic instability, pelvic fracture call will be activated, responsible general surgeons, orthopaedic surgeons, interventional radiologists, and anaesthetists will be notified to facilitate optimal assessment and actions. At the same time, a pelvic binder [10] will be applied without further delay to achieve temporary pelvic volume control and mechanical stability. Diagnostic procedures which can be carried out within minutes, including trauma series, focused assessment with sonography for trauma (FAST) or diagnostic peritoneal lavage (DPL) are used to rule out concomitant injuries.
If the focused assessment with sonography for trauma (FAST) or diagnostic peritoneal lavage (DPL) are grossly negative, patients who respond to initial resuscitation will undergo computer tomography, while the non-responders will go to the operation theatre directly without further delay by unnecessary investigations.
As time went by, there were increasing evidences that retroperitoneal pelvic packing was an effective mean to control venous bleeding, the protocol was modified as shown in Figure 2.
Figure 2: Current local protocol for management of haemodynamically unstable pelvic fracture.
On arrival to the operation theatre, the pelvic binders are kept during preparation and anaesthetization until the patients are ready for surgical interventions. The patients first undergo pelvic external fixation by anterior frame and/or C-clamp [11], followed by retroperitoneal pelvic packing and finally angio-embolization. This is the 3-in-1 pelvic damage control protocol.
The goal is to proceed to damage control surgery [12] without delay by unnecessary investigations and transport.
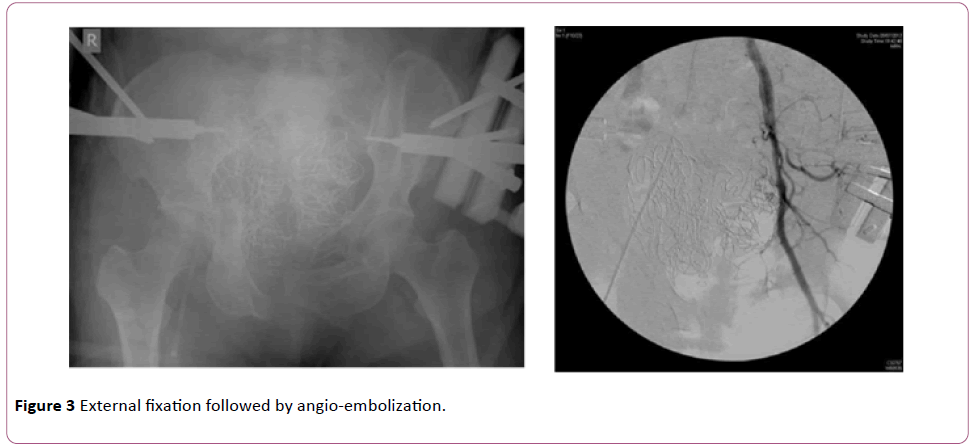
It is believed that conducting the above three procedures can optimize control of the three different sources of bleeding within the golden hour. All the above are carried out in the same theatre in an orderly manner Figure 3.
For patients with grossly positive FAST or DPL, we keep the pelvic binders over the fractured pelvis and perform laparotomies for intra-abdominal injuries first. For concomitant skeletal injuries over the limbs, further damage control surgeries are performed after stabilization of pelvic and intra-abdominal injuries.
The survival rates among the three phases were compared. The demographic data, injury severity score (ISS) and actual survival were studied.
We use the trauma and injury severity score (TRISS) to predict the outcome, which is based on the major trauma outcome study (MTOS) in the 1980s which provide data for comparison. The definitive outcome-based evaluation is used to compare the group of patient in this research and that in the database. Z-statistic defines whether the difference in outcome is statistically significant. W-score describes the differences between actual survivor in the research and the expected survivors based on the MTOS (W-score of one indicates that one extra patient out of 100 patients treated survived compared with the expected outcome out of 100 patients). M-score match the injury severity, a value closer to one indicates a better fit.
Results
From 1st January 1996 to 31st December 2015, 210 patients with haemodynamically unstable pelvic fractures were admitted into our hospital.
The survival improved from 27% in phase I (1996-2001) with external fixation alone, to 57% in phase II (2002-June 2008) with added angio-embolization, and to 71% in Phase III (July 2008 onwards) with the latest protocol. The overall survival rate was 59.52%.
Previous publication had shown that the survival rate improved from 31% to 66% since the establishment of the latest protocol in Phase III (p<0.05) [13].
We observed a continuous improving trend over the years within Phase III with continuous fine-tuning of the protocol. The survival rates in 2013, 2014 and 2015 reach 75%, 76% and 81% respectively Figure 4.
Within Phase III, the male to female ratio was 1:1.12, with a mean age of 52 (Standard deviation 22, Range 10-99). In 95% of the patients the causes of injury were fell from height or road traffic accident.
The mean ISS was 41.38 (Standard Deviation 14.62, range 5-75). The ISS is an independent factor affecting thirty days’ mortality (p<0.05).
According to TRISS, the W-score reaches 2.5 in 2014, which is statistically significant (Z score >1.96, M<0.88).
Discussion
Management of pelvic fractures had long been a challenging task. The association with haemodynamic instability and its associated injuries [14] pose combined effect to its high mortality.
The latest local protocol is based on the belief that, out of the three potential bleeding sources, the bony and venous sources are accountable for 85% in exsanguinating pelvic fracture. Thus, a timely haemorrhagic control targeting on these sources by external fixation, and retroperitoneal packing respectively should be conducted first in the acute setting within the first 30 minutes in the theatre.
Angio-embolization is complementary [15] and is followed in the same session. It is placed last because major arterial bleeding is only accountable for 15% and the procedure takes longer time to prepare and execute.
The major limitation of this study is that it is a retrospective study with a small sample size. Only 210 patients were included over near two decades.
We postulate that the improvement in survival within the latest Phase III is a result of
• improved in dedication and co-ordination through teamwork
• early and appropriate use of pelvic binder
• enhanced medical treatment of bleeding: massive transfusion protocol (MTP) and Transamin Protocol [16]
• increased early and appropriate use of C-clamp, and
• additional support from ICU
We see no statistically significant data due to the isolated effects of these factors. The genuine contribution, if any, is yet to be supported by more data in the future follow-up study.
Conclusion
To conclude, the multidisciplinary protocol established in our hospital yields improving survival over the years for patients with hemodynamically unstable pelvic fractures.
The 3-in-1 pelvic damage control protocol, with theoretically appropriate and logical arrangement of external fixation followed by retroperitoneal packing then angio-embolization builds the foundation of the improved patient survival.
References
- Khanna P, Phan H, Hardy AH, Nolan T, Dong P (2012) Multidisciplinary Management of Blunt Pelvic Trauma. Semin Intervent Radiol 29: 187-191.
- White CE, Hsu JR, Holcomb JB (2009) Hemodynamically unstable pelvic fractures. Injury 40: 1023-1030.
- Tucker MC, Nork SE, Simonian PT, Routt ML Jr (2000) Simple anterior pelvic external fixation. J Trauma 49: 989-994.
- Osborn PM, Smith WR, Moore EE, Cothren CC, Morgan SJ, et al. (2009) Direct retroperitoneal pelvic packing versus pelvic angiography: a comparison of two management protocols for hemodynamically unstable pelvic fractures. Injury 40: 54-60.
- Tai DK, Li WH, Lee KY, Cheng M, Lee KB, et al. (2011) Retroperitoneal pelvic packing in the management of hemodynamically unstable pelvic fractures: a level I trauma centre experience. J Trauma 71: E79-86.
- Cook RE, Keating JF, Gillespie I (2002) The role of angiography in the management of haemorrhage from major fractures of the pelvis. J Bone Joint Surg [Br] 84-B: 178-182.
- Lopez PP (2007) Unstable pelvic fractures: the use of angiography in controlling arterial hemorrhage. J Trauma 62: S30-31.
- Biffl WL, Smith WR, Moore EE, Gonzalez RJ, Morgan SJ, et al. (2001) Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. AnnSurg 233: 843-850.
- Cheng M, Cheung MT, Lee KY, Lee KB, Chan SC, et al. (2015) Improvement in institutional protocols leads to decreased mortality in patients with haemo- dynamically unstable pelvic fractures. Emerg Med J 32: 214-220.
- Spanjersberg WR, Knops SP, Schep NW, van Lieshout EM, Patka P, et al. (2009) Effectiveness and complications of pelvic circumferential compression devices in patients with unstable pelvic fractures: A systematic review of literature. Injury 40:1031-1035.
- Heini PF, Witt J, Ganz R (1996) The pelvic C-clamp for the emergency treatment of unstable pelvic ring injuries. A report on clinical experience of 30 cases. Injury 27: SA38-45.
- Taeger G, Ruchholtz S, Waydhas C, Lewan U, Schmidt B, et al. (2005) Damage control orthopedics in patients with multiple injuries is effective, time saving, and safe. J Trauma 59: 408–416.
- Ip KC, Lee KB (2014) Standardised multidisciplinary protocol for haemodynamically unstable pelvic fractures. J Ortho Surg 22: 1771-1780.
- Poole GV, Ward , EF, Muakkassa FF, Hsu HS, Griswold JA, et al. (1991) Pelvic fracture from major blunt trauma. Outcome is determined by associated injuries. Ann Surg 213: 538-539.
- Agolini SF, Shah K, Jaffe J, Newcomb J, Rhodes M, et al. (1997) Arterial embolization is a rapid and effective technique for controlling pelvic fracture hemorrhage. J Trauma 43: 395-399.
- Spahn DR, Cerny V, Coats TJ, Duranteau J, Fernandez-Mondeja E, et al. (2007) Management of bleeding following majo trauma: A European guideline. Crit Care 11: R17.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences