Hormonal, Metabolic and Radiological Markers of Subclinical Atherosclerosis in Egyptian Children with Type 1 Diabetes
Hoda A Atwa, Hassan A. Shora* and Amal Elsayed
Faculty of Medicine, Suez Canal University, Egypt
- *Corresponding Author:
- Hassan A. Shora
Senior Researcher, Faculty of Medicine
Suez Canal University, Egypt
E-mail: shora_hassan@hotmail.com
Received date: August 22, 2018; Accepted date: October 03, 2018; Published date: October 10, 2018
Citation: Atwa HA, Shora HA, Elsayed A (2018) Hormonal, Metabolic and Radiological Markers of Subclinical Atherosclerosis in Egyptian Children with Type 1 Diabetes. Rep Endocr Disord Vol.2 No.1:
Abstract
Endothelial dysfunction may be a critical early target for preventing atherosclerosis and cardiovascular disease. Leptin/adiponectin ratio can serve as a clinical marker of endothelial dysfunction in children with type 1 diabetes. We investigated the relationship between leptin/adiponectin ratio with carotid intima-media thickness cIMT and endothelial dysfunction in 68 type 1 diabetic children mean age 8-14 years compared to 68 healthy control subjects matched for age, sex and body mass index. A serum level of leptin was measured via radioimmunoassay and adiponectin level was measured using an enzyme linked immunosorbent assay. Flow Mediated Dilatation was significantly correlated with leptin 9.906 ± 1.688 ng/dl and leptin/adiponectin L/A ratio r -0.301, p=0.079 but not with adiponectin. Statistically significant correlation was found between carotid intima media thickness and L/A ratio (r-0.274 P=0.026), leptin (r- 0.302 P=0 .012) and adiponectin (r -0.301 P=0.079). BMI was strongly statistically correlated with cIMT. CIMT, FMD, L/A ratio, and BMI may be useful surrogate markers of subclinical atherosclerosis that make early preventive interventional strategies feasible in type 1 diabetic children.
Keywords
Endothelial dysfunction; Leptin adiponectin ratio; Carotid intimamedia thickness; Type 1 diabetes; Children
Introduction
Type 1 diabetes (T1DM) affects approximately 3 million people in the USA of whom approximately 200,000 are children [1]. The prevalence of T1DM among pediatric patients has increased between 2001 and 2009 in the USA and worldwide [2,3]. Evidence indicates that atherosclerosis begins in childhood with the accumulation of lipids in the intima of arteries to form fatty streaks [4] nearly all children have at least some degree of aortic fatty streaks by 3 years of age [5] and these fatty streaks increase after 8 years [6]. There is a growing interest to prevent the cardiovascular disease risk factors early in the course of the disease, even at pediatric stages [7]. Furthermore, endothelial dysfunction precedes the development of atherosclerosis and is believed to play a crucial role in its pathophysiology. Autopsies have shown that the atherosclerotic process at the endothelial level begins in childhood and progress rapidly in the presence of risk factors [8]. Two recent studies have demonstrated that vascular remodeling and neointimal formation are markedly attenuated in leptin deficient ob/ob mice and db/db mice with leptin receptor mutation [9,10] suggesting that leptin may accelerate the development of vascular injury. Conversely, studies with adiponectin-deficient mice have revealed that adiponectin plays a protective role in the development of atherosclerosis [11,12]. We, therefore, hypothesize that the leptin-to-adiponectin ratio serves as an atherogenic index superior to leptin or adiponectin alone compared to carotid intima-media thickness CIMT and brachial flow-mediated dilatation FMD as established clinical markers of atherosclerosis in African Egyptian type 1 diabetic children.
Materials and Methods
This study was a case-control study. It was performed on 68 of children and adolescents with type 1 diabetes mellitus attending the Pediatric Clinic of Ismailia General Hospital, Ismailia. The study was conducted during the period from 1/5/2016 to 1/2/2017. Sixty eight healthy children age and sex matched were included as control group. All children were normotensive, normoalbuminuric and had no retinopathy. Those who receive regular medications that can affect carotid intima-media thickness such as aspirin, cholesterol lowering drugs as well as children with liver and renal diseases were excluded. Height, weight, and body mass index were measured according to the Egyptian growth curves. Good glycemic control was defined as average annual HbA1C <7% and poor glycemic control average HbA1C >9%. All study groups were treated with basal bolus insulin regimen. Ethical committee of the hospital approved the study.
Laboratory investigation
Lipid profile: Venous blood samples were taken in the morning, after an overnight fast 10-12 h. Serum total cholesterol and triglyceride concentrations were measured using standard enzymatic methods [13]. Glycosylated hemoglobin (HbA1c) was determined by quantitative colorimetric determination of glycohemoglobin in whole blood [14]. Adiponectin was measured by enzyme linked immunosorbent assay (ELISA). AviBion Human adiponectin enzyme-linked immunosorbent assay kits were used for monitoring serum adiponectin level. Leptin was measured by ELISA technique, using Active Human Leotin ELISA Kit (Diagnostic Systems Laboratories, Inc., USA).
Carotid artery studies
Doppler ultrasound on carotid artery using a Philips HD11, linear array probe 12 MHz The estimation of cIMT was done at radiology department, Suez Canal University Hospital. The child was in supine position. The same experienced doctor scanned all the children, and he used the same equipment. He was blinded to study subjects concerning their clinical and laboratory characteristics. All studies were done following a predetermined, standardized scanning protocol for the right and left carotid arteries, using images of the far wall of the distal common carotid arteries and carotid bulbs according to the Mannheim common carotid IMT consensus [15]. Each CCA segment was measured. Four measurements of the intima–media thickness were averaged, in order to give the mean common carotid intima– media thickness for each side.
Flow mediated vasodilatation (FMD) of brachial artery
All children were fasted for more than 4 hours before the examination. Brachial artery diameter was assessed by a single experienced radiologist. He used an automated, beat by beat image processing software package (Vascular Tools 4.6, Medical Imaging applications, USA). The child right arm was comfortably immobilized in the extending position, allowing for ultrasound scanning of the brachial artery 5-10 cm above the antecubital fossa. Recording of vessel images were followed by inflation of a cuff to suprasystolic pressure (40-50 mmHg above systolic pressure) for 5 minutes. After the 5 minutes occlusion, the cuff was rapidly deflated to allow for reactive or flow-mediated hyperemia. Pulse wave amplitudes were recorded for at least 5 minutes after cuff was deflated [16,17].
Data analysis
All the data were collected and were statistically analyzed using SPSS 14 program. Numerical data were expressed as mean ± SD. Non-numerical data were expressed as percentage. The mean was compared using the unpaired Student’s t test. P value <0.05 was considered statistically significant. Pearson correlation was calculated to determine univariate relationships. Multiple regression analysis was performed to determine predictive variables for carotid IMT.
Ethical consideration: This study was performed with parental consent and after approval of Ismailia General Hospital ethical committee.
Results
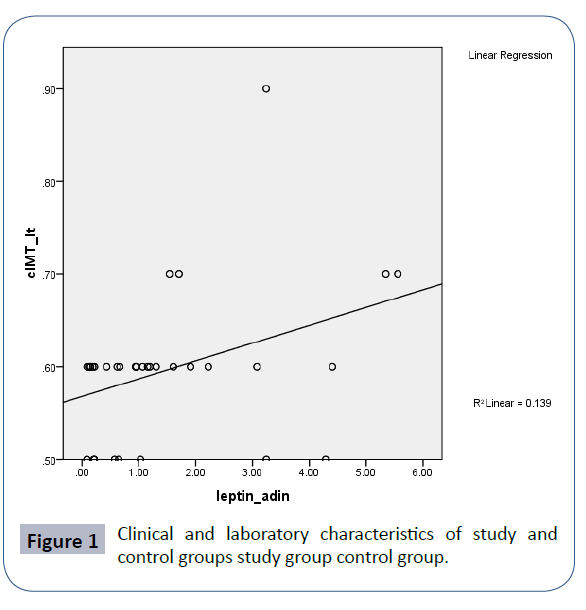
Sixty eight diabetic children their mean age was (12.15 ± 2.92 years). The mean duration of diabetes was (5.35 ± 2.19 years). The mean BMI was (20.8 ± 2.15) the mean HbA1C (8.35 ± 2.92). There was no significant difference between the study and the control group regarding their age, weight and BMI. Adiponectin level was significantly lower in children with T1DM (9.906 ± 1.68) than control (11.23 ± 1.14) (P 0.02). Children with T1DM had significantly higher cIMT (0.597 ± 0.07) than control (0.42 ± 0.045) (P 0.001). FMD was significantly lower in children with type 1 diabetes (5.097 ± 01.38) than in control (7.2 ± 1.34). Flow Mediated Dilatation was significantly correlated with leptin (r=-0.299, p=0.013) and leptin/adiponectin L/A ratio (r-0.301, P 0.079) but not with adiponectin (r163, p 191). Statistically significant correlation was found between carotid intima media thickness and L/A ratio, leptin and adiponectin (r-.274, p 0.002), (r- 302, p 0.012), (r -0.301, p 0.079) respectively. BMI was strongly statistically correlated with cIMT as well as HbA1c HbA1c r -0.33 0.79 (Figure 1).
Discussion
The combination of measuring leptin-to-adiponectin L:A ratio and CIMT might effect more atherosclerotic changes than would leptin or adiponectin alone. This study demonstrated statistically significant relationship between L:A ratio and CIMT regardless of BMI. Dalla Poza et al. found similar findings [18]. However, there was evident strong statistically significant relationship between L:A ratio and BMI in young type1 diabetic children. Leptin has peripheral actions to stimulate vascular inflammation, oxidative stress and vascular smooth muscle hypertrophy [19]. In endothelial cells, leptin stimulates transforming growth factor beta 1 synthesis [20]. The ability of leptin to promote proinflammatory signaling through cytokines and growth factors may contribute to endothelial dysfunction, atherosclerosis and insulin resistance in hyperleptinemic states [21]. Ouchi et al. found that endothelium-dependent vasorelaxation was impaired in subjects with low plasma adiponectin concentration [22]. A recent study has also demonstrated that adiponectin attenuates high glucose-induced production of reactive oxygen species in endothelial cells through a cAMP-PKA-dependent mechanism. This study demonstrated a strong significant association between elevated HbA1c levels and cIMT. Thus, activation of cAMP-PKA signaling is an important mechanism by which adiponectin protects endothelial cells from activation. Developing an inhibitor to cAMP-PKA is at experimental investigations and may be future effective treatment. Adenovirus-mediated supplementation of adiponectin inhibits the formation of atherosclerotic lesions and decreases mRNA levels of SR-A, TNF-α and VCAM-1 in the vascular wall [23]. Adiponectin acts as an important regulator of endothelial nitric oxide synthase (eNOS), a key determinant of endothelial function and angiogenesis. Adiponectin promotes eNOS phosphorylation in endothelial cells through AMP-activated protein kinase (AMPK)-dependent signaling mechanisms [24]. Adiponectin also prevents apoptosis in endothelial cells through activation of AMP signaling [25]. Adiponectin suppresses production of cytokines like TNF∞ by macrophages, suppresses accumulation of lipids in monocytes derived from macrophages and inhibits transformation of macrophages into foam cells [26]. Furthermore adiponectin participates in the stabilization of atherosclerotic plaques by increasing expression of tissue inhibitor of metalloproteinase1 TIMP1 in infiltrating macrophages [27]. Taken together, these favorable actions of adiponectin on endothelial function and vessel growth could contribute to vascular protection [28]. Observational studies in children showed an inverse correlation between plasma adiponectin concentrations, adiposity, and insulin resistance [29,30], hepatic fat by magnetic resonance imaging [31-35], and carotid intimamedia thickness [36]. Satoh et al. reported that plasma L:A ratio is correlated with pulse wave velocity [37]. Brachial Flow- Mediated dilatation was significantly correlated with leptin 9.906 ± 1.688 ng/ml and adiponectin r-0.327, P= 0.055 and L:A ratio as well r-0.301 P = 0.079. Brachial flow-mediated dilation (FMD) is a measure of the release of nitric oxide by the endothelium due to a transient flow stimulus. Impaired brachial FMD is widely regarded as an early and potentially reversible manifestation of vascular disease and may represent an integrated measure of the impact of various insults to the endothelium [38]. Diabetes is another chronic medical condition known to impair vascular function in children [39]. Decreases in both FMD and NED (Nitroglycerin Enhanced Dilatation) have been observed in children with type 1 diabetes mellitus [40]. Ja¨rvisalo et al. studied 105 healthy children and found that peak FMD was 7.7_4.0% in attempt to reach normative value of FMD. FMD is an indirect measure of endothelial dysfunction [41]. However, the technique measures the vascular changes associated with atherosclerosis, has been widely used and validated in children, shows strong dose-response associations with known cardiovascular risk factors, and in older subjects predicts clinical cardiovascular risk [42]. New guidelines of International Society of Pediatric Endocrinology and Diabetes emphasized screening and treatment of cardiovascular risk factors in diabetic children at age 11 years. Folate supplementation improved endothelial dysfunction in folate deficient diabetic children [43]. SEARCH CVD study included 402 T1D patients of average age 10-22 years, demonstrated higher cIMT of carotid bulbs compared to healthy controls [44]. A recent meta-analysis of 90 studies that included 2656 confirmed that T1D patients had a significantly greater cIMT (SMD: 0.89; 95% CI, 0.69-1.09; P< .001), significantly lower FMD% (SMD:_1.45%; 95% CI, _1.74 to _1.17; P< .001), significantly increased cf-PWV (SMD: 0.57; 95% CI, 0.03-1.11; P< .001), and significantly decreased GTN% (SMD: _1.11; 95% CI, _1.55 to _0.66; P< .001) than controls [45]. Furthermore, a recent study protocol of a large critical review and meta-analysis to detect risk factors and determinants of carotid intima-media thickness in children with prenatal and postnatal environmental exposure is ongoing [46]. Hyperglycemia is the major casual factor in the development of endothelial dysfunction in diabetes [47]. A highly significant correlation is found between HbA1c and L:A ratio along with CIMT and FMD. The latter has been demonstrated in recent studies to be decreased and reliable marker of endothelial dysfunction in patients with risk factors for atherosclerosis [48-50].
Conclusion
Our study suggests that L:A ratio, CIMT FMD and HbA1c can serve as clinical non-invasive reliable markers of endothelial dysfunction and subclinical atherosclerosis in children with type 1 diabetes. Clinicians could use those markers as diagnostic and prognostic mentoring tools for primary prevention of cardiovascular diseases where potential therapeutic interventions are feasible.
References
- CDC (2014) National Diabetes Statistics Report.
- Dabelea D, Davis EJM, Saydah S, Imperatore G, Linder B, et al. (2014) Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 311: 1778-1786.
- Patterson CC, Gyurus E, Rosenbauer J, Cinek O, Neu A, et al. (2012) Trends in childhood type 1 diabetes incidence in Europe during 1989-2008: evidence of non-uniformity over time in rates of increase. Diabetologia 55: 2142-2147.
- Berenson GS (1986) Evolution of cardiovascular risk factors in early life: perspectives on causation. In Causation of Cardiovascular Risk Factors in Children: Perspectives on Cardiovascular Risk in Early Life. Berenson GS, Raven Press, New York pp: 1-26.
- Krishnan P, Balamurugan A, Urbina E, Srinivasan SR, Bond G, et al. (2003) Cardiovascular risk profile of asymptomatic healthy young adults with increased carotid artery intima-media thickness: the Bogalusa Heart Study. J La State Med Soc 155: 165-169.
- Singh TP, Groehn H, Kazmers A (2003) Vascular function and carotid intimal-medial thickness in children with insulin-dependent diabetes mellitus. J Am Coll Cardiol 41: 661-665.
- Punthakee, ZDelvin, EO’LoughlinJ (2006) Adiponectin, Adiposity, and Insulin Resistance in Children and Adolescents. J Clin Endocrinol Metab 91: 2119-2125.
- Rodriguez R, Omez DG, Tanus Haj (2007) Carotid Intima-Media Thickness in Pediatric Type 1 Diabetic Patients. Diabetes Care 30: 2599-2602.
- Donoso M, M Barrios, Garrido G, Hawkins F, Argente J (2010) Increased circulating adiponectin levels and decreased leptin/soluble leptin receptor ratio throughout puberty in female ballet dancers: association with body composition and the delay in puberty. Eur J Endocrinology 162: 905-911.
- Stephenson K, Tunstead J, Tsai A, Gordon R, Henderson S, et al. (2004) Neointimal formation after endovascular arterial injury is markedly attenuated in db/db mice. Arteriosclerosis Thrombi Vasc Biol 23: 2027-2033.
- Kavey RE, Allada V, Daniels SR (2006) Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation 114: 2710-2738.
- Scha¨fer K, Halle M, Goeschen C (2004) Leptin promotes vascular remodeling and neointimal growth in mice. Arterioscler Thromb Vasc Biol 24: 112-117.
- Marshall, Tanner JM (1968) Growth and physiological development during adolescence. Ann Rev Med 19: 283.
- Myher J, Kuksis A, Breckenridge W, Little J (1984) Studies of triacyglycerol structure of very low density lipoproteins of normolipemic subjects and patients with type III and type IV hyperlipoproteinemia. Lipids 19: 683-691.
- Gabbay KH, Hasty K, Breslow JL (1977) Glycosylated haemoglobins and long term blood glucose control in diabetes mellitus. J Clin Endocrinol Metab 44: 859-64.
- Touboul PJ, Hennerici MG, Meairs S (2007) Mannheim carotid intima-media thickness consensus (2004-2006). An update on behalf of the advisory board of the 3rd and 4th watching the risk symposium 13th and 15th European stroke conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis 23: 75-80.
- Corretti MC, Anderson TJ, Benjamin EJ (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 39: 257-265.
- Dalla PR, Netz H, Schwarz HP, Bechtold S (2010) Subclinical atherosclerosis in diabetic children: results of a longitudinal study. Pediatr Diabetes 11: 129-133.
- Kubota N, Terauchi Y, Yamauchi T, Kubota T, Moroi M, et al. (2002) Disruption of adiponectin causes insulin resistance and neointimal formation. J Biol Chem 277: 25863-25866.
- Matsuda M, Shimomura I, Sata M, Arita Y, Nishida M, et al. (2002) Role of adiponectin in preventing vascular stenosis: the missing link of adipo-vascular axis. J Biol Chem 277: 37487-37491.
- Giannini C, Giorgis D, Scarinci T, Cataldo A, Marcovecchio IM, et al. (2009) Increased carotid intima-media thickness in pre-pubertal children with constitutional leanness and severe obesity: the speculative role of insulin sensitivity, oxidant status, and chronic inflammation. Eur J Endocrinology 161: 73-80.
- Ouchi N, Kihara S, Arita Y (1999) Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein adiponectin. Circulation 100: 2473-2476.
- Kobashi C, Urakaze M, Kishida M (2005) Adiponectin inhibits endothelial synthesis of interleukin-8. Circ Res 97: 1245-1252.
- Ouchi N, Kihara S, Arita Y (2000) Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation 102: 1296-1301.
- Ouedraogo R, Wu X, Xu SQ (2006) Adiponectin suppression of high-glucose-induced reactive oxygen species in vascular endothelial cells: evidence for involvement of a cAMP signaling pathway. Diabetes 55: 1840-1846.
- Kumada M, Kihara S, Ouchi N (2004) Adiponectin specifically increased tissue inhibitor of metalloproteinase-1 through interleukin-10 expression in human macrophages. Circulation 109: 2046-2049.
- Okamoto Y, Kihara S, Ouchi N (2002) Adiponectin reduces atherosclerosis in apolipoprotein E-deficient mice. Circulation 106: 2767-2770.
- Ouchi N, Kobayashi H, Kihara S (2004) Adiponectin stimulates angiogenesis by promoting cross-talk between AMP-activated protein kinase and Akt signaling in endothelial cells. J Biol Chem 279: 1304-1309.
- Chen H, Montagnani M, Funahashi T, Shimomura I, Quon MJ (2003) Adiponectin stimulates production of nitric oxide in vascular endothelial cells. J Biol Chem 278: 45021-45026.
- Kobayashi H, Ouchi N, Kihara S (2004) Selective suppression of endothelial cell apoptosis by the high molecular weight form of adiponectin. Circ Res 94: e27-e31.
- Lin LY, Lin CY, Su TC, Liau CS (2004) Angiotensin II-induced apoptosis in human endothelial cells is inhibited by adiponectin through restoration of the association between endothelial nitric oxide synthase and heat shock protein 90. FEBS Lett 574: 106-110.
- Satoh N, Naruse M, Usui T (2004) Leptin-to-Adiponectin Ratio as a Potential Atherogenic Index in Obese Type 2 Diabetic Patients. Diabetes Care 710: 2488-2490.
- Bacha F, Saad R, Gungor N, Arslanian SA (2004) Adiponectin in youth: relationship to visceral adiposity, insulin sensitivity, and beta-cell function. Diabetes Care 27: 547-552.
- Sinaiko AR, Steinberger J, Moran A (2005) Relation of body mass index and insulin resistance to cardiovascular risk factors, inflammatory factors, and oxidative stress during adolescence. Circulation 111: 1985-1991.
- Cambuli VM, Musiu MC, Incani M, Paderi M, Serpe R, et al. (2008) Assessment of adiponectin and leptin as biomarkers of positive metabolic outcome after lifestyle intervention in overweight and obese children. J Cli Endocrinol Metab 93: 3051-3057.
- Burgert TS, Taksali SE, Dziura J (2006) Alanine aminotransferase levels and fatty liver inchildhood obesity: associations with insulin resistance, adiponectin, andvisceral fat. J Clin Endocrinol Metab 91: 4287-4294.
- Joannides R, Haefeli WE, Linder L, Richard V, Bakkali EH, et al. (1995) Nitric oxide is responsible for flow-dependent dilation of human peripheral conduit arteries in vivo. Circulation 91: 1314-1319.
- Widlanksy ME, Gokce N, Keaney JF, Vita JA (2003) The clinical implications of endothelial dysfunction. J Am Coll Cardiol 42: 1149-1160.
- Celermajer DS, Sorensen KE, Gooch VM (1992) Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 340: 1111-1115.
- Libby P, Ridker PM, Maseri A (2002) Inflammation and atherosclerosis. Circulation 115: 1135-1143.
- Ja¨rvisalo MJ, Raitakari M, Toikka JO, Putto-Laurila A, Rontu R, et al. (2004) Endothelial dysfunction and increased arterial intima-media thickness in children with type 1 diabetes. Circulation 109: 1750-1755.
- Sass C, Herbeth B, Chapet O, Siest G, Visvikis S, et al. (1998) Intima-media thickness and diameter of carotid and femoral arteries in children, adolescents and adults from the Stanislas cohort: effect of age, sex, anthropometry and blood pressure. J Hypertens 16: 1593-1602.
- Donaghue (2018) ISPAD Clinical Practice Consensus Guidelines 2018 Microvascular and macrovascular complications in children and adolescents.
- Urbina EMD, D’Agostino RB Jr, Shah AS, Dolan LM, Hamman R, et al. (2013) Effect of type 1 diabetes on carotid structure and function in adolescents and young adults: the SEARCH CVD study. Diabetes Care 36: 2597-2599.
- Epure AM, Leyvraz M, Mivelaz Y (2018) Risk factors and determinants of carotid intima media thickness in children: protocol for a systematic review and meta-analysis.
- Wang P, Xu Y, Lv T, Guan S, Li X, et al. (2018) Subclinical Atherosclerosis in Patients With Type 1 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Angiology pp: 1-19.
- Ja¨rvisalo MJ, Ro¨nnemaa T, Volanen (2002) Brachial artery dilatation responses in healthy children and adolescents. Am J Physiol Heart Circ Physiol 282: H87-H92.
- Ross R (1993) The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 362: 801-809.
- Slyper AH (2004) Clinical Review: What vascular ultrasound testing has revealed about pediatric atherogenesis, and a potential clinical role for ultrasound in pediatric risk assessment. J Clin Endocrinol Metab 89: 3089-3095.
- Mullen MJ, Thorne SA, Deanfield JE (1997) Noninvasive assessment of endothelial function. Heart 4: 297-329.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences