Congenital Anomalies Presenting to a Tertiary Neonatal Intensive Care Unit: A Descriptive Study
1John Hunter Children’s Hospital, Locked Bag 1, Hunter Region Mail Centre NSW 2310, Australia
2Hunter Genetics, PO Box 84, Waratah NSW 2298, Australia
3School of Medicine, University of Newcastle, Newcastle, NSW, Australia
- *Corresponding Author:
- Dulani Siddhisena
Hunter Genetics, PO Box 84, Waratah NSW
2298, Australia
Tel: +61 4985 3100
E-mail: Dulani.Siddhisena@hnehealth.nsw.gov.au
Received date: August 20, 2018; Accepted date: August 29, 2018; Published date: September 04, 2018
Citation: Siddhisena D, Goel H. Congenital Anomalies Presenting to a Tertiary Neonatal Intensive Care Unit-A Descriptive Study. J Birth Defects 2018, 1:2
Copyright: © 2018 Siddhisena D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Congenital anomalies are becoming an increasingly important contributor towards paediatric morbidity as a consequence of improved survival and higher standards of care.
Aims: To examine the various congenital anomalies admitted to a tertiary neonatal intensive care unit, focusing on sociodemographic factors, resources utilized, and short-term outcome.
Methods: A retrospective study was undertaken through examining medical records of all babies admitted with congenital anomalies to the Neonatal Intensive Care Unit (NICU) of John Hunter Children’s Hospital, NSW, from 2005 to 2015. Socio-demographic details and antenatal risk factors were evaluated. A descriptive analysis was done on the various presenting anomalies and their secular trends. The duration of intensive care as well as average cost were inspected. Finally, an evaluation was done on the short-term outcome of these babies in terms of mortality, discharge from NICU or transfer to another hospital.
Results: There were 891 admissions with congenital anomalies, with a prevalence rate of 76.15 per 1000 admissions. The male to female ratio was 1.5:1. Most mothers were aged between 25 and 29 years of age, and in most this was their first pregnancy. There was an increase in trend of admissions over the years. Most congenital anomalies involved the cardiovascular system, followed by digestive system anomalies. The mean length of stay was 19.71 days. The majority of deaths were in association with a cardiovascular anomaly. A significant proportion of babies were transferred to other hospitals for specialized or continued care.
Key Words
Congenital anomalies; Neonate; Burden of care; New South Wales
What is already known on this topic?
• Congenital anomalies contribute significantly towards paediatric morbidity.
• Understanding the prevalence of various congenital anomalies is important for planning resource allocation.
• There are limited studies on the burden of care posed by congenital anomalies.
What this study adds.
• There is an increasing trend of admissions for certain congenital anomalies, particularly cardiovascular anomalies.
• There is considerable impact on antenatal and neonatal resources required for these neonates.
• The nature of common anomalies implies considerable effects on long-term morbidity.
Introduction
A congenital anomaly is defined as a structural or functional anomaly that occurs during intrauterine life, and can be identified prenatally, at birth or later in life [1]. The World Health Organization estimates that 276,000 babies die every year worldwide as a result of such anomalies [1]. Beneath the tip of this iceberg there is bound to be a vast impact, not only on morbidity and health resources, but also on the unmeasurable impacts upon each individual child and family.
In New South Wales, Australia, the rate of congenital conditions varied from 18.1 to 20.7 per 1000 babies during 2004 to 2009 [2]. A reported 20,983 babies had some form of congenital anomaly between 2004 and 2010, of which the majority (28%) were due to anomalies in the cardiovascular system, followed by congenital defects in the musculoskeletal system which amounted to 19.9% [2].
When considering the principal causes of death in the paediatric population, it is evident that conditions surrounding birth are the greatest contributors, of which congenital anomalies play a significant role. Between 2004 and 2013, maternal, neonatal and congenital causes amounted to more than half of the total deaths in the paediatric population of New South Wales [3]. Of the five leading causes of deaths in neonates in NSW, congenital anomalies were second (22%), with ‘conditions arising in the perinatal period’ being the leading cause (71%) [4].
We studied the prevalence and socio-demographic characteristics of congenital anomalies being admitted to intensive care, and the impact on health resources.
Methods
A retrospective survey was done of all babies admitted to the Neonatal Intensive Care Unit of John Hunter Children’s Hospital with a diagnosis of congenital anomalies. This tertiary centre caters to babies born within the hospital as well as accepting a significant proportion of transfers from local hospitals in the Hunter New England region of New South Wales.
The study period was January 2005 to December 2015. The NICUS database, which is a collaborative data collection of babies admitted to specified neonatal intensive care units in New South Wales and Australian Capital Territory, was utilized to generate an output of data for all cases meeting the main inclusion criteria.
The inclusion criteria for the study: Babies born of a gestational age of greater than 24 weeks and admitted to the Neonatal Intensive Care Unit, and having a structural or functional anomaly which occurred during intrauterine life, and which was diagnosed antenatally and/or within the first 28 days of life were included in our study.
The average daily cost of care was calculated based on Diagnosis Related Group (DRG) calculations derived from the NICUS database for a random representative sample from our study population.
Statistical analysis
SPSS (Statistical package for Social Sciences) version 22 was utilized to derive descriptive statistical values. Microsoft excel was utilized to generate most charts and graphs. Prevalence rates were calculated per 1000 total admissions.
Results
There were 891 admissions with congenital anomalies to the Neonatal Intensive Care Unit of John Hunter Children’s Hospital between 2005 and 2015, corresponding to a period prevalence of 76.15 per 1000 admissions. The study population consisted of 534 males and 357 females, equivalent to a male: female ratio of 1.5:1. The majority of admissions (57.5%) were term babies, although a significant proportion (28.2%) was between of 32 and 36 weeks’ gestational age. Only 4.1% of admissions were in the extreme premature category of <28 weeks’ gestation.
There were 341 babies who were in the low birth weight category (less than 2500 grams), accounting for 38.3% of the total study population.
Maternal age, parity and previous preterm deliveries
Most mothers of babies admitted with a congenital anomaly were aged between 25 and 29 years (28.9%). There were 162 mothers (18.2%) aged above 35 years, with three of these women being above 45 years of age. The overall NSW rate for mothers above 35 years of age was 24.2% in 2010 [2].
There were 7.6% of mothers in the teenage age group. This is a higher rate compared to overall NSW rates of teenage mothers in 2010, which was 3.3% in 2010 [2].
In 256 (28.7%) mothers, this was their first pregnancy, whereas in 76 mothers (8.5%), there had been 5 or more previous pregnancies. The majority of women reported either one or two previous pregnancies. Previous miscarriages were reported in 113 (12.7%) of mothers in the study population.
Maternal health and pregnancy related illnesses
Gestational diabetes mellitus was reported in 75 (8.4%) pregnancies. This compares to overall New South Wales rates ranging from 5.6% to 7.5% between 2010 and 2014 [5]. Hypertension during pregnancy was seen in 105 (11.8%) mothers, whereas NSW rates during 2010-2014 ranged from 2.8%-2.9% [5].
The common indications for induction and/or delivery are depicted in Table 1. The diagnosis of fetal congenital anomaly was a cause for induction or delivery in almost 20% of pregnancies.
| Presenting problem | Number | Percentage |
|---|---|---|
| Preterm pre-labour rupture of membranes | 66 | 7.4 |
| Preterm labour | 133 | 14.9 |
| Antenatal diagnosis of fetal anomaly | 174 | 19.5 |
| Suspected IUGR | 50 | 5.6 |
| Hypertension in pregnancy | 39 | 4.4 |
| Fetal distress | 47 | 5.3 |
| Antepartum haemorrhage | 21 | 2.4 |
| Other | 361 | 40.5 |
Table 1: Presenting problem necessitating induction and/or delivery of babies with a Congenital Anomaly
Diagnosis of fetal anomaly
An antenatal diagnosis of the congenital anomaly had been made in 402 neonates, accounting for 45.23% of instances. In-utero detection rates (compared to non-detection rates) were higher in anomalies of the central nervous system, as well as respiratory anomalies, orofacial clefts, abdominal wall defects, and urinary tract anomalies.
Description of congenital anomalies
All cases in the study population had been coded as per the International Classification of Diseases Version 10 [6].
The European Surveillance of Congenital Anomalies (EUROCAT) guidelines were utilized to classify each congenital anomaly as a major or minor anomaly, as well as to assign them to the clinical system involved as per the EUROACT subgroup of congenital anomalies [7].
From the 891 patients studied, 582 babies had a single anomaly, whereas 170 had a combination of 2 anomalies (although this could have been related to the same clinical system, such as different congenital cardiac lesions or intestinal malformations). 62 babies had a combination of three anomalies. There were 77 neonates with a combination of 4 or more anomalies, with a maximum of 10 anomalies recorded in a single patient.
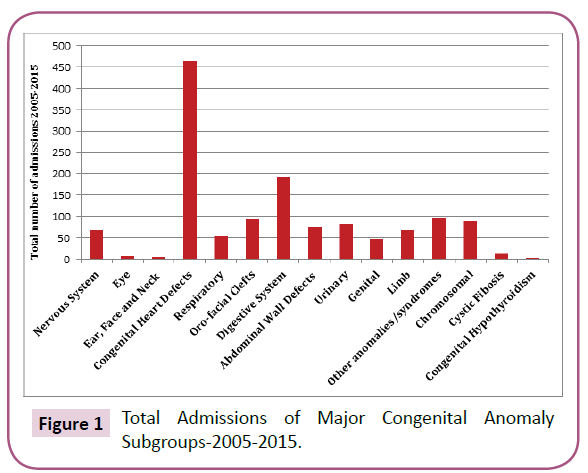
The majority of patients had major malformations, with a total number of 1353 malformations being recorded in the study population. There were 81 minor malformations reported. Figure 1 provides an overview of the frequencies of major congenital anomalies identified in our study population. Table 2 lists common anomalies as per the EUROCAT guidelines.
| Nervous System | 67 |
| Corpus callosum agenesis | 10 |
| Microcephaly | 7 |
| Lumbar spina bifida with hydrocephalus | 4 |
| Spina bifida without hydrocephalus | 4 |
| Hydrocephalus | 2 |
| Eye | 6 |
| Ear, Face and Neck | 5 |
| Congenital Heart Defects | 463 |
| VSD | 122 |
| ASD | 92 |
| Patent Ductus Arteriosus‡ | 39 |
| Coarctation of Aorta | 38 |
| Tetralogy of Fallot | 23 |
| AVSD | 19 |
| Pulmonary valve atresia/stenosis | 16 |
| Pulmonary artery atresia/stenosis | 12 |
| DORV | 9 |
| Aortic stenosis/atresia | 8 |
| TAPVD | 5 |
| Hypoplastic left heart | 5 |
| Ebstein anomaly | 5 |
| Respiratory | 55 |
| Hypoplasia and dysplasia of lung | 11 |
| Congenital cystic lung | 10 |
| Choanal atresia | 7 |
| Sequestration of lung | 4 |
| Oro-facial Clefts | 94 |
| Cleft lip with or without cleft palate | 57 |
| Cleft palate | 37 |
| Digestive System | 191 |
| Diaphragmatic hernia | 32 |
| Oesophageal atresia with or without TOF | 31 |
| Atresia or stenosis of other parts of small intestine | 24 |
| Duodenal atresia or stenosis | 19 |
| Hirschsprung's disease | 19 |
| Anorectal atresia and stenosis | 17 |
| TOF without oesophageal atresia | 4 |
| Abdominal Wall Defects | 75 |
| Gastroschisis | 55 |
| Exomphalos | 20 |
| Urinary | 82 |
| Congenital hydronephrosis | 18 |
| Posterior urethral valves | 7 |
| Polycystic kidney | 3 |
| Cystic renal dysplasia | 3 |
| Genital | 47 |
| Hypospadias | 39 |
| Limb | 67 |
| Club foot-Talipes Equinovarus | 39 |
| Syndactyly | 9 |
| Polydactyly | 6 |
| Other anomalies/syndromes | 97 |
| VATER/VACTERL | 12 |
| Beckwith Weideman syndrome | 5 |
| Noonan syndrome | 4 |
| Prader-Willi syndrome | 2 |
| Osteogenesis imperfecta | 2 |
| Congenital cytomegalovirus infection | 2 |
| Chromosomal | 88 |
| Down syndrome/Trisomy 21 | 53 |
| Klinefelter syndrome | 4 |
| Turner syndrome | 2 |
†Only the common anomalies have been described in italic form below each subgroup, and adding the numbers of these anomalies will not equal to the total number of each subgroup due to omission of less common anomalies. ‡Only Patent Ductus Arteriosus anomalies found in neonates beyond 37 weeks’ gestational age were included in the analysis, as per EUROCAT guidelines. VSD, Ventricular Septal Defect; ASD, Atrial Septal Defect; AVSD, Atrioventricular Septal Defect; DORV, Double Outlet Right Ventricle; TAPVD, Total Anomalous Pulmonary Venous Circulation; TOF, Tracheo-Oesophageal Fistula; VATER, Vertebral, Anal, Tracheal (O) Esophageal Renal malformations; VACTERL, Vertebral, Anal, Cardiac, Tracheal, (O) Esophageal, Renal, Limb malformations.
Table 2: Frequencies of major congenital anomalies†.
It is evident that cardiac anomalies are the commonest, accounting for 33.2% of total anomalies. Amongst the various congenital cardiac anomalies, ventricular septal defects were the commonest (26.3%). There were 53 neonates with Trisomy 21, which accounted for 62.5% of all chromosomal anomalies.
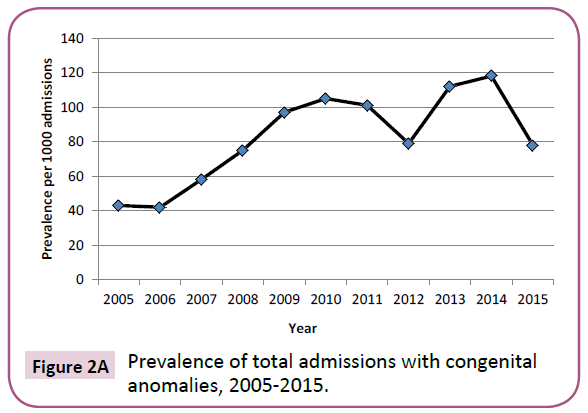
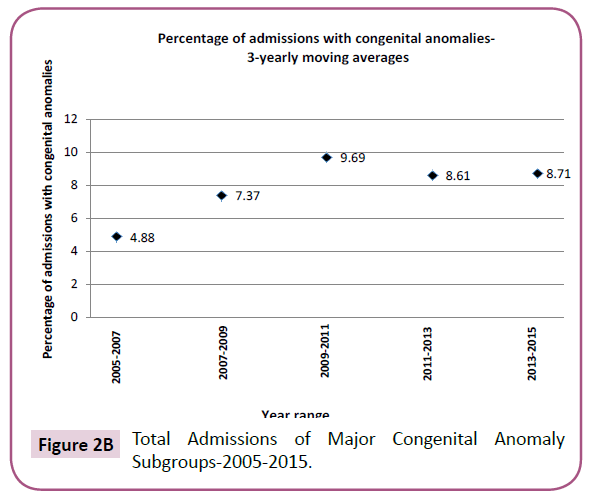
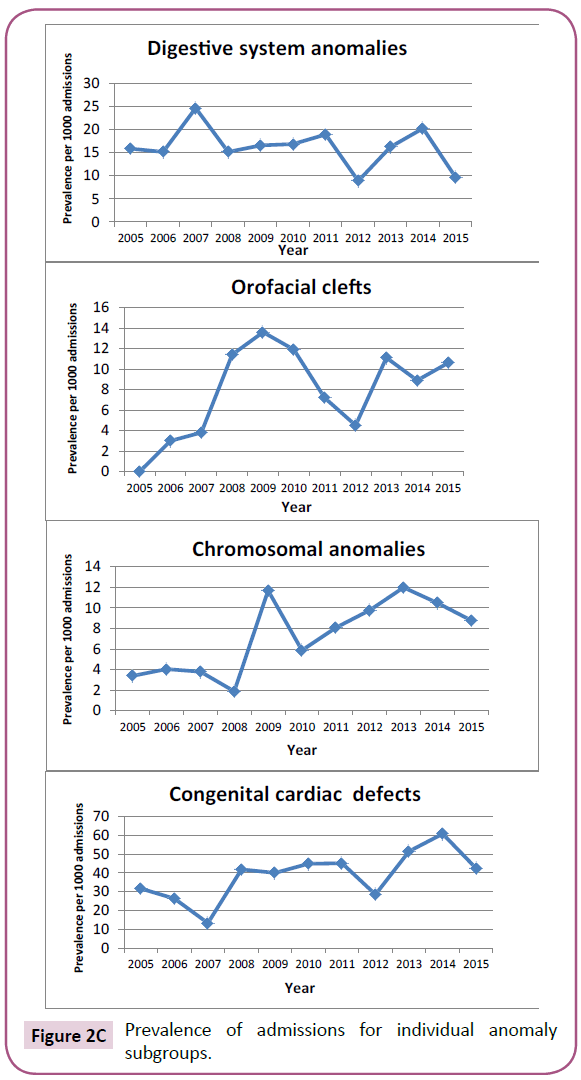
The trend of admissions for neonates with congenital anomalies is illustrated in Figure 2, depicting the total prevalence trend, as
well as trends for anomalies of certain individual clinical systems.Resource utilization
The mean length of stay was 19.71 days, and there was a range of 0.04 to 211.6 days. The mode was 3.71 days. The average daily cost of care estimated for this subgroup of neonates was 25, 890.67 AUD per neonate.
Outcome
Amongst 891 neonates studied, there were 67 deaths recorded by the time of discharge or separation from the unit (This does not reflect the number of babies who may have died at a later stage or following transfer to another hospital).
A cardiac abnormality was associated in 17 deaths (25.4%). Respiratory causes such as hypoplasia or dysplasia of the lungs were seen in 8 deaths (11.9%). There were 9 babies who had abdominal wall defects (Gastroschisis or Omphalocoel), accounting for a death rate of 12% amongst all neonates in this subgroup. Other digestive tract anomalies were seen in another 9 deaths. Amongst the deaths, the majority (45) had a single anomaly, whereas in 22 neonates more than one anomaly was documented.
507 babies had been transferred to other hospitals for specialized care (such as cardiac surgery), or continuation of care.
Discussion
Studies of congenital anomalies are of value as not only do they depict population trends, but may also be helpful for us to understand potentially causative and modifiable genetic and environmental factors. Understanding the prevalence of these disorders is also important for planning resource allocation throughout the lifespan of these children.
Our study obviously depicts a very selective population of neonates admitted for highly specialised care, and this would not reflect the true prevalence of congenital anomalies in the general population. However, this study sample does provide a glance at the characteristics of some of the sickest babies with congenital anomalies in the region, who were admitted to the leading tertiary centre for management.
When comparing the gestational age and birth weights of neonates in the study population with overall NSW health statistics during the corresponding time period [8], it is evident that there is a larger proportion of neonates in the late preterm category of 32-36 weeks’ gestation (28.2% vs. 6.05%), as well as low birth weight categories of <2500 grams (38.3% vs.5.9%). This would independently increase requirements for higher standards of neonatal care, in addition to the resources required to manage individual birth defects. An analysis of the mode of delivery in this subgroup also highlights the need for higher levels of obstetric care. There is a higher percentage of babies being delivered through instrumental (25.7%) and emergency caesarean deliveries (31.2%) compared to corresponding NSW health statistics (11% and 12.5% respectively) [8].
Comprehensive data was not available regarding the prevalence of alcohol use, smoking, recreational drug use, and other environmental risk factors. This is a major limitation in our medical records, and a standardized template for record keeping would be useful to study potential environmental associations.
An evaluation of individual birth defects and their trends of admission reveal an increasing trend in most anomalies (Figures 2A-2C). Although this may reflect a lower threshold towards admission with increased detection rates and awareness, it does not obscure the fact that increasing resources are required for providing care to these babies in a NICU setting.
Congenital heart defects took precedence over all other birth defects. The vast majority were septal defects, which may or may not have been in combination with other more serious structural heart defects. Anomalies of the gastrointestinal system, the second commonest in our study population, mainly involved diaphragmatic hernias, tracheoesophageal fistulae, and small intestinal atresia/stenosis.
Long-term health implications of these major birth defects should be taken into consideration when planning resource allocation. Twenty-year survival rates for individuals with congenital diaphragmatic hernia have been estimated to be 57.1% based on a study done by Tennent et al. [9]. Similar regional studies of survival would therefore complement prevalence studies and provide an approximation of the morbidity and mortality expected in these individuals beyond the neonatal period.
Information from this study would also be useful in further research to identify potentially causative genetic and environmental factors for common congenital anomalies, which would thereby enable consideration of prevention strategies.
Finally, as a means of studying birth defects in a more comprehensive and precise manner, we would like to highlight the importance of maintaining comprehensive regional and national registries for congenital anomalies, not only recording live-births, but also miscarriages, stillbirths and terminations of pregnancy, where a diagnosis was made antenatally or following autopsy.
Limitations of This Study
This study was conducted on a potentially biased sample, and may not reflect the true incidence and prevalence of congenital anomalies in the region. A larger study utilizing state-wide data obtained from congenital anomaly registers, which, in addition to stillbirths and terminations of pregnancy, would also include neonates who did not require admission to a NICU or special care nursery, would be important to gain a more comprehensive assessment.
Although data were presented regarding the antenatal diagnosis of congenital anomalies, we were not able to ascertain the exact gestational age when these diagnoses were made. The differences in prevalence of individual anomalies may reflect the behaviour of parents, as well as potential medical influences towards decision making with regards to termination of pregnancies, particularly if detected after 20 weeks’ gestation. More comprehensive data on maternal smoking, alcohol, medication and recreational drug use would have been useful in ascertaining patterns of anomalies related to potentially teratogenic substances.
Acknowledgements
The authors would like to thank Lynne Cruden, data manager, Neonatal Intensive Care Unit of John Hunter Children’s Hospital, for her immense contribution towards complication of the data required for this study. We would also like to thank Dr Paul Craven, Director of Newborn Services, for his support and approval to utilize data from the NICUS database. No external funding was utilized for this study.
Ethical Approval
Obtained from the Hunter research ethics committee on 15/12/2015.
References
- WHO (2015) World Health Organization factsheets April 2015.
- Centre for Epidemiology and Evidence (2012) New South Wales Mothers and Babies 2010. Sydney: NSW Ministry of Health.
- Centre for Epidemiology and Evidence. Health Statistics New South Wales. Sydney: NSW Ministry of Health.
- NSW child death review team (2014) NSW Ombudsman. Annual Report.
- Centre for Epidemiology and Evidence (2014) New South Wales Mothers and Babies.
- WHO (2002) International Statistical Classification of disease and related health problems 10th revision: version for 2002.
- EUROCAT (2012) Data Collection. Malformation Coding Guides. Coding of EUROCAT subgroups of Congenital Anomalies: Chapter 3.3, Guide 1.4.
- NSW Perinatal Data Collection (SAPHaRI). Centre for Epidemiology and Evidence, NSW Ministry of Health.
- Tennant WG, Pearce MS, Bythell M, Rankin J (2010) 20-year survival of children born with congenital anomalies: a population-based study. Lancet 375: 649-656.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences