A Low-Cost Customizable Prosthetic Foot with Energy Return Capabilities
Department of Engineering, University of Texas, El-Paso, Texas, USA
- *Corresponding Author:
- Joshua Bowen, M.S
Graduated Master's student
Department of Engineering, University of Texas
El-Paso, Texas, USA
Tel: 1-530-990-2453
E-mail: bowenjosh@gmail.com
Received date: November 14, 2017; Accepted date: January 01, 2018; Published date: January 08, 2018
Citation: Bowen J, Hausselle J, Gonzalez R (2018) A Low-Cost Customizable Prosthetic Foot with Energy Return Capabilities. Pros Orth Open J 2:1.
Copyright: © 2018 Bowen J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Energy storage and return prosthetic feet
improve the mobility of lower-limb amputees but prosthetic
solutions available in the Under-Developed World do not
meet the needs of active amputees.
Case description and methods: This study aimed at
developing and testing a hand-manufactured low-cost
modular prosthetic foot with energy-return capabilities.
Carbon fiber layers of varying stiffness were assembled to
construct the toe section. Static tests were performed to
measure the overall foot stiffness and ensure that our
prototype withstands proof and ultimate loads. Two
unilateral amputees performed gait trials to assess the
prototype’s behaviour during gait.
Findings and outcomes: Interchangeable toe layers enabled
the prototype’s stiffness to vary between 31 and 40 N/mm,
to withstand proof and ultimate ISO loads, and to return
about 70% of the energy stored during loading. Two
amputees tested the foot and were able to maintain
temporal gait parameters within 10% of the values
measured when using their own prosthetic feet.
Conclusion: This study confirmed the feasibility of handmanufacturing
a low-cost modular composite fibre
prosthetic foot with energy return capabilities.
Keywords
Prosthetic; Feet; Energy return; Modular; Low cost
Introduction
Limb amputations have tremendous consequences on the amputee’s autonomy. While energy storage and return energy prosthetic feet are rarely seen in the Under-Developed World, effective implementation of dynamic response feet would greatly benefit working amputees.
Losing a foot due to amputation has tremendous consequences on the patient’s quality of life and autonomy. Amputees exhibit significant changes of several biomechanical and physiological gait parameters such as walking speed, muscle activity, gait symmetry, and energy expenditure [1]. Prosthetic limbs are therefore designed to restore biomechanical functionality while minimizing adverse effects such as gait asymmetry [2-4].
However, prosthetic limb technology in the Developed World (DW) has significantly outpaced technology in the Under- Developed World (UDW) [5,6], where nearly 30 million amputees have limited access to reliable prosthetic devices [6]. Prosthetic technology specifically designed for and available in the UDW often does not meet international test standards and fail to meet specific challenges of the UDW, especially regarding reliability, reparability, and patient-specificity [7].
Energy storage and return (ESAR) prosthetic feet are designed to replicate the function of the ankle plantar flexors [8] by storing energy during the first midstance phase of the gait cycle and releasing energy during the push-off phase [8]. Although biomechanical analyses comparing ESAR to passive feet did not show significant differences regarding temporal gait parameters [9-11] and ground reaction forces [12,13], patients perceive increases in velocity and stability [14]. The few ESAR feet available in the UDW cannot easily be adapted to patient specific needs and repaired without specific tools.
ESAR feet available to amputees in the UDW are either donated second hand DW prosthetic feet or the Niagara foot. Donated components from the DW do not perform well in the UDW since they are not designed to deal with the rugged conditions and the amount of physical work to be performed by amputees. The increased distances traveled and heavier loads applied to prosthetic components in the UDW due to manual labor tasks necessitate particularly robust prosthetic feet [15].
The Niagara foot is an injection molded Delrin core that can be covered with a rubber cosmesis and costs approximately $35 [16]. The foot was developed for active users in rugged conditions and has been field-tested in South America [17]. Analyses found that patients increased their cadence and reduced their stride length when walking with the Niagara versus the SACH foot [17].
The Niagara’s updated version of their injection molded foot is patient-specific, which means the Delrin core can be shaved down to accommodate for patient’s height and needs in terms of energy return capabilities. However, any alteration is permanent and testing of the Niagara foot’s mechanical properties have only been carried out on its standard core, therefore potential effects of any geometrical modifications on the foot’s behavior and lifespan are unknown.
Since the Niagara foot is injection-molded, its production process requires expensive machinery, thus limiting the production locations and by extension the deployment and availability of the Niagara foot. In addition, it is only offered in a single size and can only be adapted to smaller-than-average amputees. To overcome the limitations inherent to ESAR technology in the UDW, this study aimed at developing and testing a hand-manufactured, low-cost, modular prosthetic foot. Following the historical development of ESAR feet, the toe section of the prosthetic foot was the primary focus, as well as passing static ISO standard tests [18].
Case Description and Methods
Case studies
Two patients were recruited to test the effect of our prototype prosthetic foot on gait biomechanics. Patient 1 was an active 45-year-old transtibial unilateral amputee (1.73 m, 73.3 kg) in good health and no medical complications. Patient 2 was an active 50-year-old transfemoral unilateral amputee (1.80 m, 89.8 kg) also in good health and no medical complications. A licensed prosthetist fitted and aligned the prosthetic foot and was present during data collection. Prior to testing, approval was received from the Institutional Review Board and patients provided informed consent [19].
Prototype development
The prototype prosthetic foot (PPF) design mimicked an Össur Vari-Flex [20] size 27, category 4, prosthetic foot provided by LIMBS International (El Paso, Texas). Category 4 rates the foot for moderate impact levels for patient weighing 69-77 kilograms, which is typical of an amputee in the UDW. The prosthetic foot was manufactured from plain weave 3k carbon fiber fabric (Soller Composites, LLC; NH, USA) and laminated together with 820 epoxy with medium hardener (AdTech, OK, USA). Composite components were manufactured with compression molds in aluminium, cured, cut out, and sanded to final size.
Mechanical characterization
We used force-deflection tests to measure the stiffness of individual layers and the assembled PPF per the ISO 10328 standard [21], with the toe and heel sections oriented at 20° and 15°, respectively. Static proof and ultimate tests were performed with a PPF assembled with three layers (stiff, soft, and intermediate); as this configuration was a good overall representation of the average PPF response. The toe section was loaded at a rate of 0.063 mm/sec up to a deflection of 25.4 mm, and subsequently unloaded. The stiffness was calculated based on the load measured at 25.4 mm of deflection. Deflection was limited to prevent any damage to the PPF.
The energy storage capacity was assessed by integrating the loading and unloading curves. ISO 10328 static proof and ultimate tests [16,17] were performed to P4 test levels, which simulate loads based on a maximum patient weight of 80 kilograms. The toe section was oriented at 20° and forces were applied at 0.063 mm/s up to 2065 N for the proof test and 3098 N for the ultimate test. A fatigue test was performed until failure per ISO 22675 at P4 loads, with forces of 1158 N applied at the toe and 1173 N at the heel. One PPF was used for each to the ISO tests, i.e. static proof, static ultimate, and fatigue. At the conclusion of each static test and throughout the fatigue test, the PPFs were visually inspected for signs of delamination and potential cracks.
Biomechanical analyses
When fitted with the PPF, patients were given time to adapt. They were instructed to walk at a comfortable self-selected speed that could be sustained throughout the session and performed ten 10-meter gait trials with their standard prosthetic foot (SPF), and ten trials with the PPF. Patient 1’s SPF was an Ossur Vari-Flex and Patient 2’s SPF was an Ossur Ceterus. They first walked across a force plate (AMTI, MA, USA) that recorded ground reaction forces (GRF) at 120Hz, and then across a GAITRite Mat (GAITRite, NJ, USA) that computed step length, stride length, cadence, and velocity.
Braking and propulsive energies were assessed by integrating the positive and negative parts of the antero-posterior GRF, respectively. All the variables were averaged over ten trials. Intra-subject comparisons were performed using unpaired ttests and differences were considered significant for p-values below 0.05. Following trials, patients answered a questionnaire involving comparing heel strike and toe-off sensations, weight, comfort, perceived energy usage, and ability to walk with the PPF in comparison with their SPF.
Findings and outcomes
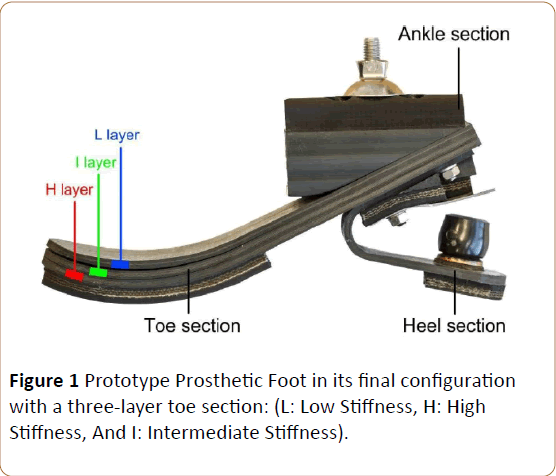
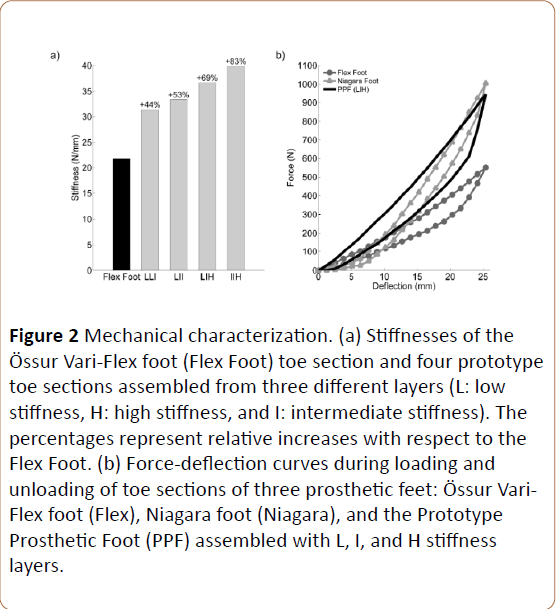
Prototype development and mechanical characterization: A size 27 category 4 PPF was manufactured using approximately $73.00 (USD) of materials and twelve man-hours. Three interchangeable toe layers with different stiffness levels were manufactured and assembled to build the PPF (Figure 1). Stiffness values of the three toe layers varied from High (H) (22.6 N/mm), Intermediate (I) (13.7 N/mm), and Low (L) (11.2 N/mm). This novel design approach allowed us to combine different toe layers to achieve an overall foot stiffness that varied from 31 N/mm to 40 N/mm (Figure 2) [19].
Figure 2: Mechanical characterization. (a) Stiffnesses of theÖssur Vari-Flex foot (Flex Foot) toe section and four prototype toe sections assembled from three different layers (L: low stiffness, H: high stiffness, and I: intermediate stiffness). The percentages represent relative increases with respect to the Flex Foot. (b) Force-deflection curves during loading and unloading of toe sections of three prosthetic feet: Össur Vari-Flex foot (Flex), Niagara foot (Niagara), and the Prototype Prosthetic Foot (PPF) assembled with L, I, and H stiffness layers.
The hysteresis curve of a PPF assembled with L, I, and H layers showed that the foot returned about 69% of the mechanical energy. PPF withstood the static proof and ultimate tests with no visual damage. Measurements before, during, and after fatigue testing showed no decrease of the overall PPF stiffness and, after 100,000 fatigue cycles, no signs of delamination or damage were visible.
However, cracks were observed after 150,000 cycles at the location of maximum curvature of the toe section. The handmanufacturing was a key design criterion to produce an ESAR prosthetic foot that could be manufactured on site without the need of specialized tools. Since the composite material can be worked using similar methods to woodworking, it is a good candidate to empower local manufacturing [20,21].
The modular design allows the PPF to be assembled or modified without returning to the clinic to alter the alignment of the prosthesis. This is especially beneficial for users in UDW countries who live far from the cities [7]. Previous studies on ESAR prosthetic feet found energy loss ranging from 18% to 31% [22]. The energy loss of the PFF lies in the upper range, which indicates that the design could be improved to provide additional energy return. Tuning the PPF to return the appropriate amount of energy with the correct timing will be an important next step in the development of the foot since Hafner et. al. [12,14] highlighted that this timing affects the walking speed.
Results and Discussion
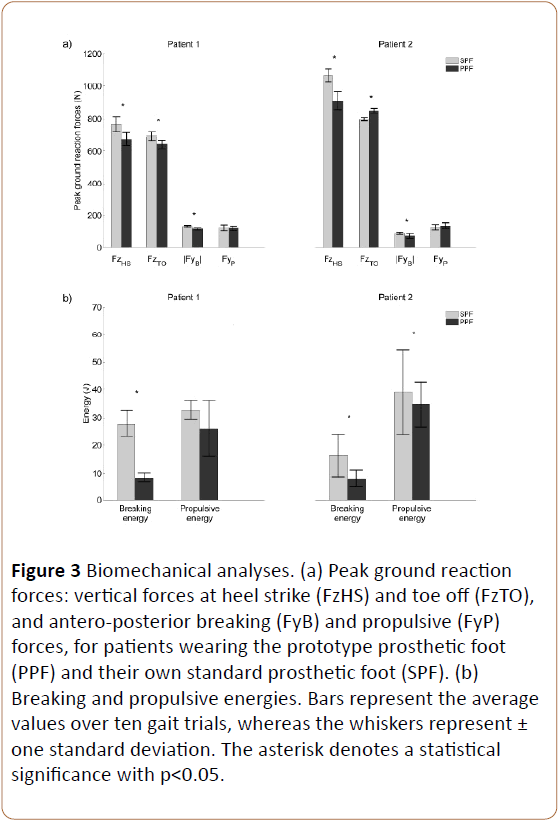
Mean peak vertical forces and peak breaking horizontal forces significantly decreased (p<0.05) for both patients when wearing the PPF (Figure 3). Vertical peak forces decreased for Patient 1 and 2 by 12% and 15% at heel strike and 8% and 6% at toe off, respectively; whereas braking horizontal peak forces decreased by 12% and 17%. Similarly, mean braking and propulsive energies significantly changed (p<0.05) when wearing the PPF (Figure 3).
Figure 3: Biomechanical analyses. (a) Peak ground reaction forces: vertical forces at heel strike (FzHS) and toe off (FzTO), and antero-posterior breaking (FyB) and propulsive (FyP) forces, for patients wearing the prototype prosthetic foot (PPF) and their own standard prosthetic foot (SPF). (b) Breaking and propulsive energies. Bars represent the average values over ten gait trials, whereas the whiskers represent± one standard deviation. The asterisk denotes a statistical significance with p<0.05.
Breaking energies decreased by 67% and 47% for Patient 1 and 2, respectively; whereas propulsive energy decreased by 9% for patient 1 and increased by 8% for patient 2. Regarding temporal gait parameters, only the stride length of the amputated side significantly decreased (p<0.05) for both patients when wearing the PPF (Table 1). However, all temporal parameter changes when wearing the PPF versus the SPF remained below 6%. Analysis of answers to the post-test questionnaire showed that both patients found the toe stiffness of the PPF adequate.
| Parameters | Patient 1 | Patient 2 | ||
|---|---|---|---|---|
| SPF | PPF | SPF | PPF | |
| Step Length (cm) | 78.7 (1.9) | 79.0 (1.6) | 78.8 (0.8) | 74.3 (2.0)* |
| Stride Length (cm) | 152.2 (2.6) | 149.1 (3.1)* | 145.6 (1.7) | 141.7 (3.0)* |
| Capedence (step/minute) | 106.8 (3.6) | 106.2 (3.1) | 93.8 (1.1) | 96.4 (1.3)* |
| Velocity (cm/s) | 134.5 (5.2) | 132.7 (1.7) | 114.9 (6.0) | 113.3 (2.1) |
Table 1 Patient data.
Walking with the PPF compared to their STF, changes measured were comparable to values observed from altering the stiffness of ESAR feet. Stride length, cadence, and velocity were within patients’ inter-session variations observed previously. Other studies comparing ESAR feet with conventional feet showed virtually no change in velocity and cadence [8]. No biomechanical changes when patients walk with different prosthetics is considered a good outcome since previous studies have only found slight variations and highlighted that benefits of ESAR feet are captured in the qualitative response of patients. Both patients noted that the PPF was lighter and less stiff than their own prosthetic feet, which reflected in the reduction of the propulsive force recorded during gait. This may primarily stem from the fact that patients’ prosthetic feet were rated for extreme activities. The present study only focused on the toe part of the foot, which is not the part that stores energy during the first mid-stance phase. This can explain the high end energy loss measured. Future work will focus on developing a modular heel section to improve the energy storage and release capacities. These improvements will be critical to allow the amputee to regain a smoother and more symmetric gait pattern. In addition, while our prototype passed the ISO static tests, further refinement is needed for the PPF to pass the ISO fatigue test to achieve a minimum lifetime of three years. Since previous work has shown that modern composite prosthetic feet can pass ISO fatigue tests with no issues [23], we are confident in our ability to achieve similar results. Once the mechanical requirements are met, we will focus on on-site testing in UDW countries such as Bangladesh or Ecuador to ensure that our foot meets specific field criteria. Finally, further deployment will also require adapting the prosthetic to cultural cosmetic requirements.
Conclusion
We proved the feasibility of developing a low-cost, modular, energy return composite prosthetic foot for the UDW. The PPF designed passed ISO Static test while allowing the stiffness to be patient-specific and the components to be replaceable without the need to realign the prosthesis. The modularity of the PPF also enables field repairs and maintenance to occur without the need for a prosthetist, which benefits patients living in rural areas.
References
- Sagawa Y, Turcot K, Armand S (2011) Biomechanics and physiological parameters during gait in lower-limb amputees: A systematic review. Gait Posture 33: 511–526.
- Meanley S(1995) Different approaches and cultural considerations in third world prosthetics. Prosthet Orthot Int 19: 176–180.
3. Strait E (2006) Prosthetics in developing countries. The american academy of orthotists and prosthetists, USA. - Ventura JD, Klute GK, Neptune RR (2011) The effects of prosthetic ankle dorsiflexion and energy return on below-knee amputee leg loading. Clin Biomech 26: 298–303.
- https://usatoday30.usatoday.com/money/industries/health/2007-07-15-prosthetics_N.htm
- https://haitiamputees.nbcnews.com/_news/2010/03/20/4040341-limb-loss-a-grim-growing-global-crisis
- Cummings D (1996) Prosthetics in the developing world: A review of the literature. Prosthet Orthot Int 20: 51–60.
- Postema K, Hermens FU, Vries J (1997) Energy storage and release of prosthetic feet, part 1: Biomechanical analysis related to user benefit. Prosthet Orthot Int 21: 17–27.
- Torburn L, Perry J, Ayyappa E (1990) Below-knee amputee gait with dynamic elastic response prosthetic feet: a pilot study. J Rehabil Res Dev 27: 369–384.
- Torburn L, Powers CM, Guiterrez R (1995) Energy expenditure during ambulation in dysvascular and traumatic below-knee amputees: A comparison of five prosthetic feet. J Rehabil Res Dev 32: 111–119.
- Goh JCH, Solomonidis SE, Spence WD (1984) Biomechanical evaluation of SACH and uniaxial feet. Prosthet Orthot Int 8: 147–154.
- Hafner BJ, Sanders JE, Czerniecki JM (2002) Transtibial energy-storageand-return prosthetic devices: A review of energy concepts and a proposed nomenclature. J Rehabil Res Dev 39: 1–11.
- South BJ, Fey NP, Neptune RR (2010) Manufacture of energy storage and return prosthetic feet using selective laser sintering. J Biomech Eng 132: 138.
- Hafner BJ, Sanders JE, Czerniecki J (2002) Energy storage and return prostheses: Does patient perception correlate with biomechanical analysis? Clin Biomech 17: 325–344.
- Sam M, Hansen AH, Childress DS (2004) Characterisation of prosthetic feet used in low-income countries. Prosthet Orthot Int 28: 132–140.
- https://www.niagarafoot.com/news/news01.html
- Gabourie R, Beshai M, Bryant T(2007) The development and production of assistive devices using a distributed network: The Niagara Foot. In: 12th World Congress of the International Society for Prosthetics and Orthotics, Vancouver, Canada.
- https://www.iso.org/standard/38708.html
- 20. Wagner J (2009) Composite material fabrication. Wolfgang Publications.
- 21. Poonekar P (1992) Prosthetics and orthotics in India. Report, national institute of child health and human development, USA.
- 22. Geil MD (2002) An iterative method for viscoelastic modeling of prosthetic feet. J Biomech 35: 1405–1410.
- 23. Craig J (2005) Prosthetic feet for low-income countries. J Prosthet Orthot 17: 47–49.
- 24. Mason ZD, Pearlman J, Cooper RA (2011) Comparison of prosthetic feet prescribed to active individuals using ISO standards. Prosthet Orthot Int 35: 418–424.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences