A Comparative Study between the Effect of Breathing Control and Pursed Lip-Breathing Exercises in COPD Patients on Expiratory Flow Rate
Snehal Potdar*
PES Modern College of Physiotherapy, Maharashtra University of Health Sciences, Pune, Maharashtra, India
- *Corresponding Author:
- Snehal Potdar
BPTH, PES Modern College of Physiotherapy
Maharashtra University of Health Sciences
Pune, Maharashtra, India
Tel: 0253-6659111
E-mail: snehalsp9773@gmail.com
Received date: August 21, 2018; Accepted date: September 20, 2018; Published date:September 30, 2018
Citation: Potdar S (2018) A Comparative Study between the Effect of Breathing Control and Pursed Lip-Breathing Exercises in COPD Patients on Expiratory Flow Rate. J Physiother Res. 2018, Vol.2 No.4:12.
Copyright: © 2018 Potdar S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The purpose of the study was to find out the effect of breathing control and pursed-lip breathing in COPD patient on expiratory flow rate by the end of 1 week. Total 30 participants (including male and female) in group A and B ranging from 45-65 were randomly selected. Peak flow meter was used to assess the effect of breathing control and pursed lip-breathing. Statistical analysis of the data was done and significant improvement in the expiratory flow rate with pursed lip-breathing (p<0.0001) was noted. Hence, these results suggest that one week, significantly improves expiratory flow rate in COPD patients.
Keywords
Breathing control; Pursed lip-breathing; COPD; Peak flow meter
Introduction
Chronic Obstructive Pulmonary Disease is a preventable and treatable disease, where airflow obstruction occurs with bronchial hyper responsiveness [1]. COPD includes the chronic bronchitis and emphysema [1]. Chronic bronchitis is characterized by chronic cough with expectoration for at least 3 months of the two consecutive years and Emphysema is defined as permanent abnormal distention of the air spaces distal to the terminal bronchioles [1]. In COPD, Chronic bronchitis and emphysema produces airways narrowing which causes breathlessness in the patient [1]. Also the lung hyperinflation occurs in the COPD, which lead to increase work of breathing, because of that breathlessness occurs in these patient [1]. COPD is a combination of airway narrowing, parenchymal destruction and pulmonary vascular thickening. Changes related to chronic airway inflammation and most pronounced to peripheral airways are due to imbalances of proteinases/anti proteinases or oxidants/antioxidants and chronic inflammation is characterized by increase in neutrophils, macrophages and T lymphocytes, damage the endothelial lining of the airways [2], Where airway damage result in airway repair, leading to airway remodeling [2]. Decrease in the ciliary function and alteration in physiochemical characteristics of the bronchial secretions also impair airways clearance and contribute to airway obstruction. In COPD, the airways are pulled open wide by thoracic expansion, allowing air to enter. So during exhalation, the airways narrowing from inflammation, remodeling and excessive secretions, causes premature closure and air trapping in the distal airways and airspaces, which causes decrease in Expiratory flow rate, especially FEV1 and ratio of FEV1 to FVC is also decreased (<70%).
In COPD patients, hyperinflation induced diaphragm shortening occurs and function of the diaphragm is disturb and reduced contractile property of the diaphragm to generate breathing forces. So the breathing control help to increase the efforts of the inspiratory muscles and recoiling of the tissues, which causes the increase in the arterial gas exchange, which helps to increase expiratory flow rate [1]. Peak flow meter is one of the most widely used instruments for monitoring patient with airway disease and its evaluation of asthma and chronic bronchitis [3]. Peak flow meter reliability and variability; total average variability for 24 patients is 15.0 × 10-2l2.S-2. Variability caused by instrumental, interpolated from standard deviation i.e., 5.61 × 10-2l2.S.2, Varinstr to Vartot=-20.37+9.88 PFFR its range from 8-100% [3]. Pursed lipbreathing is expiratory breathing exercise used mainly in obstructive condition. The mechanism behind using Pursed-lip breathing is that it keeps airways open by creating back pressure in the airways, which increase the tidal volume and reduces work of breathing which increases the expiratory flow in COPD patient [4]. Breathing control which is breathing exercise, the mechanism behind using breathing control is normal tidal breathing using the lower chest and encouraging relaxation of the upper chest and shoulder which prevents bronchospasm [5]. Which lead to increase in the expiratory flow in COPD Patient.
Materials and Methods
Methodology
Purpose: The purpose of this study to find the effect of breathing control and pursed-lip breathing on expiratory flow rate by the end of 1 week in COPD patients.
Selection of the subjects: 30 patients in group A and B each (including both males and females) ranging from 45-65 were selected randomly from nearby hospitals in Pune.
Procedure: Group A was given the Breathing Control Technique for increasing expiratory flow. Breathing control technique includes following procedure, tell the patients breathing in slowly with nose and count numbers e.g., 1, 2 etc. Then ask the patient to expire out with the nose counting e.g., 1, 2, 3, 4 etc. Count the numbers in the ratio of 2:1 (expiration: inspiration). Repeat this for 5-10 cycles. Group B; was be given the Pursed lip-Breathing Technique for increasing the Expiratory Flow. Patient assumes a comfortable position and relax as much as possible. Have the patient breath in slowly and deeply through the nose then breathe out gently through lightly pursed lip as if blowing on and bending the flame of candle, but not blowing it out. Explain the patient that expiration must be relaxed and that contraction of the abdominals must be avoided. Place therapist hands over the patient abdomen to detect any contraction of the abdominal muscle. These are repeated for 5-10 cycles.
Finding: Pre and post data was analyzed with the help of Graph Pad In stats®.
Results
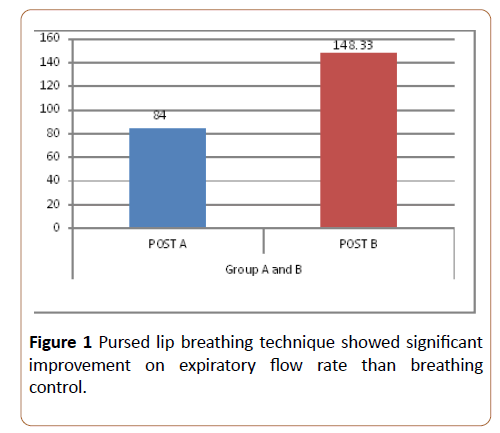
Post data showing that the p-value <0.0001 which is extremely significant and hence pursed-lip breathing is effective in improving expiratory flow rate in COPD patients (Figure 1 and Table 1).
| MEAN ± SD | t-Value | p-Value | Significance | |
|---|---|---|---|---|
| Expiratory Flow rate POST (A) | 193.67 ± 13.25 | 20.434 | <0.0001 | Significant |
| Expiratory Flow rate POST (B) | 258.33 ± 11.67 |
Table 1: Showing comparison between Breathing control and pursed lip breathing across outcome measure.
Discussion
The present study was done to see the effectiveness of breathing control and pursed-lip breathing on expiratory flow rate assessed by using peak flow meter in patient with COPD. For this study, total 60 patients both male and female were included with 30 participants in each group (breathing control and pursed lip-breathing). Study was done in and around Pune for 1 week and data was collected pre and post treatment. Expiratory flow rate was measured with peak flow meter. Later the Data was statistically analyzed using Paired t-test for outcomes within the groups and unpaired t-test for outcomes between the 2 groups. The difference between the pre and post values of both the groups was statistically analyzed which showed significance. P-value of all the outcome measures is <0.0001, t value for expiratory flow rate is 20.434. The present study results demonstrate that subjects with expiratory flow rate receiving pursed lip-breathing treatment experienced greater improvement in expiratory flow rate when compared with subjects receiving breathing control group. In this study we found that breathing control and pursed lip-breathing are effective in increasing expiratory flow rate in COPD patients. Further on, comparing breathing control and pursed lipbreathing we found that pursed-lip breathing is more effective in increasing expiratory flow rate in COPD patients.
Our results are in account with Gosselink. Kolaczkowski et al. investigated 21 patients with emphysema (forced expiratory volume in 1 s [FEV1] 40% of predicted value), the effect of a combination of relaxation exercise and manual compression of thorax in different body position. In experimental group, the excursion of the thorax and the oxygen saturation increased significantly which increases expiratory flow rate [6]. The past few studies have witnessed an increase in non-pharmacological treatment approach to expiratory flow rate, First Casciari et al. studied additional effects of active expiration during exercise training in patient with severe COPD, they observed a significantly larger increase in maximum intake oxygen uptake after a period of additional controlled breathing was added to training program. Although active expiration is common in resting breathing and during exercise in COPD patients and it seems to improve inspiratory muscle function [6]. Erpicum et al. studied the effect of active expiration with abdominal contraction on lung function parameters in patients with COPD and in healthy subjects, while functional residual capacity decreases while transdiaphragmatic pressure increased and increased elastic recoil pressure in lung tissue, which improves expiratory flow rate [6]. Breslin et al. observed that rib cage and accessory muscle recruitment increased during the entire breathing cycle of pursed lip-breathing, which found to be effective to improve gas exchange and reduced dyspnea [6]. In account with Mueller et al. reported that a lowered PaCO2 was induced by PLB in resting subjects with COLD. They then state: their data suggest that symptom benefit from PLB is related to the magnitude of respiratory rate decrease and tidal volume increase it induces [7]. These positive effects appear to be related to the technique’s ability to decrease airway narrowing during expiration, an effect attributed to decreasing the resistive pressure and helps to improve expiratory flow rate [7]. Motley’s studied (residual volume_270% predicted, vital capacity_71% predicted, maximum voluntary ventilation_32% predicted). The investigators reported that PLB slowed breathing frequency (from 19-12 breaths per minute) and that both slow, deep breathing and PLB resulted in a similar increase in Vt (from a baseline of 0.61 L to 0.82 L and 0.84 L for slow, deep breathing and PLB respectively). These changes resulted in decrease in PaCO2 (from a baseline of 55 mm Hg to 52 mm Hg and 51 mm Hg, for slow, deep breathing and PLB, respectively) that was not associated with a change in slow space volume (volume of the poorly ventilated airspaces) or functional residual capacity [7]. Hence the present study proved the alternative hypothesis (H2) i.e., Pursed-lip breathing is better treatment for improving expiratory flow rate compared to Breathing control in COPD patient. Because where it keeps airways open by creating back pressure in the airways, which increases the tidal volume and reduces work of breathing which causes increase in the expiratory flow in COPD patient as proved in Erpicum et al. study [6,8-10].
Conclusion
In this study Pursed lip-breathing treatment appeared to be more effective than breathing control technique to increase expiratory flow rate in COPD patients.
References
- Shah SN, Anand MP (2009) Eighth Edition reprint, API Textbook of Medicine.
- O’Sullivan SB, Schmitz TJ (2011) Physical rehabilitation: A handbook for researching online. FA davis company, USA.
- Schayck CPV, Dompelling E, Weel CV, Folgerin H, Hoogen HJVD (1990) Accuracy and reproducibility of the assess peak flow meter. Eur Respir J 3: 338-341.
- Kisner C, Colby LA (1996) Therapeutic Exercises: Foundations and Techniques (third edition). A handbook of researching online, FA Davis, Philadelphia, USA.
- Pryor JA, Prasad SA (2007) Physiotherapy for Respiratory and Cardiac Problems. A handbook for researching online (fourth edition). Churchill livingstone, UK.
- Gosselink R (2003) Controlled breathing and dyspnea in patients with chronic obstructive pulmonary disease (COPD). J Rehab Res Dev 40: 25-33.
- Barach AL (1973) Physiologic advantages of grunting, groaning, and pursed-lip breathing: adaptive symptoms related to the development of continuous positive pressure breathing. Bull N Y Acad Med 49: 666-673.
- Frownfelter DL, Dean EW (1996) Principles and Practice of Cardiopulmonary Physical Therapy. A handbook for researching online. St. Louis: Mosby-year book, USA.
- Jindal SK (2006) Emergence of chronic obstructive pulmonary disease as an epidemic in india. Ind J Med Res 124: 619-630.
- Gigliotti F, Romagnoli I, Scano G (2003) Breathing retraining and exercise conditioning in patients with chronic obstructive pulmonary disease (COPD): a physiological approach. Respir Med 97: 197-204.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences