PCOS 2018
Journal of Clinical and Molecular Endocrinology
ISSN: 2572-5432
Page 22
June 07-08, 2018
London, UK
4
th
World Congress on
Polycystic Ovarian
Syndrome
Introduction:
Polycystic ovarian syndrome (PCOS) affects 5
to 10% of women of reproductive age resulting in menstrual
abnormalities, hyperandrogenism, infertility, metabolic
disturbances and cardiovascular risk. We aimed to examine
the subclinical metabolic and cardiovascular features in young
women with PCOS.
Methods:
118 young women were recruited, with 15 self-
reporting a diagnosis of PCOS. Body composition was
evaluated by DEXA scan and physical fitness by VO2 max
testing. Women were assessed for blood pressure, response
to volume challenge, aortic-femoral pulse wave velocity, flow
mediated vasodilation, adrenergic response to Valsalva, as
well as uterine, renal and cardiac hemodynamics. Complete
blood counts, metabolic and lipid profiles were assessed.
Homeostatic Model Assessment of Insulin Resistance (HOMA-
IR) was calculated as an index of insulin resistance. All studies
were conducted during the follicular phase of the menstrual
cycle, or following a withdrawal bleed (mean 9.4±3.5 days).
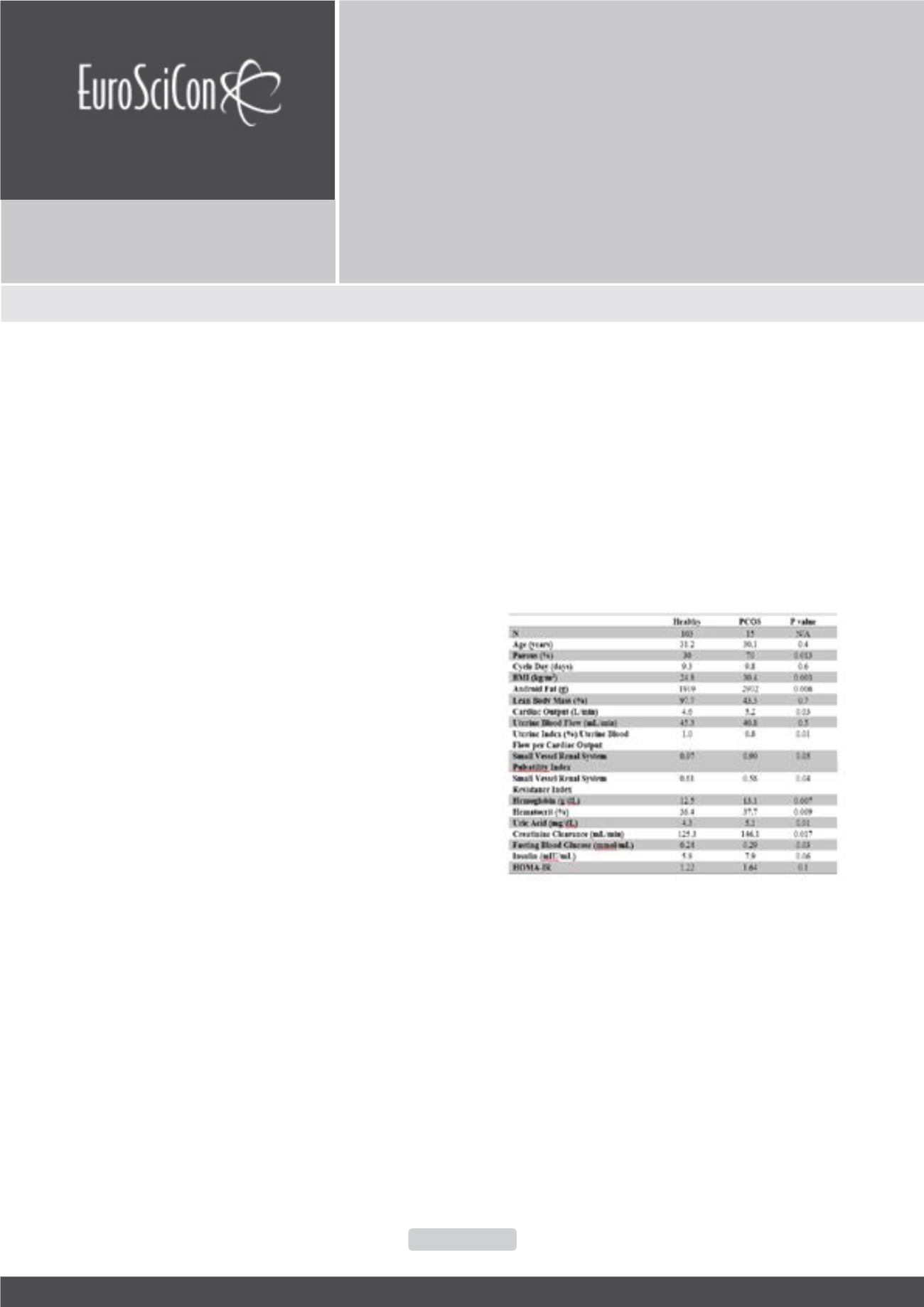
Results:
There was no difference in age between groups. We
identified differences in BMI, total fat and fat distribution, all
showing statistically significant increases in PCOS. Renal and
cardiac volumetrics, as well as laboratory markers also differed
in PCOS (Tables 1). We saw no differences between healthy
and PCOS subjects in adrenergic response, plasma volume,
blood pressure, vessel compliance in response to volume
challenge, uterine blood flow, pulse wave velocity and lipid
profile. Angiotensin II, urine sodium and creatinine statistically
differed between the two groups. Fasting glucose, insulin and
HOMA-IR trended higher in PCOS, although not all significantly.
Conclusions:
Although our sample size is small, our results
suggest that physiology of women with PCOS differs from that
of healthy women. These differences may help explain clinical
trajectories, both pregnancy related, as well as long term health
risks associated with PCOS.
Biography
Tendai M Chiware is a Reproductive Endocrinology and Infertility Fellow in
Vermont, USA. She attended medical school at the University of Birming-
ham in the UK. She was a Trainee in the UK and a member of the Royal
College of Obstetricians and Gynaecologists. She completed her Residency
in Michigan, USA and is board certified with the American Board of Obstet-
rics and Gynecology. She worked at the Department of Reproductive Health
and Research of the World Health Organization in Geneva, Switzerland. Her
interests include PCOS, Diminished Ovarian Reserve, Fertility Preservation,
Minimally Invasive Surgery, Reproductive Surgery and Global Health. She
has presented her work at national and international meetings including, the
Society for Reproductive Investigation, and she will be speaking at the Eu-
ropean Society of Human Reproduction and Embryology’s annual meeting.
Tendai.Chiware@uvmhealth.orgPrepregnancy phenotype and physiological characteristics in PCOS
Tendai M Chiware
1
, Carole McBride
1
, Elizabeth McGee
1
, Gary J Badger
2
and
Ira Bernstein
1
1
Dept. of Obstetrics, Gynecology & Reproductive Sciences
2
Medical Biostatistics
University of Vermont College of Medicine, USA
Tendai M Chiware et al., J Clin Mol Endocrinol 2018, Volume 3
DOI: 10.21767/2572-5432-C1-002
Table 1:
Demographics of renal and cardiac volumetric,
and laboratory markers