Keywords
Infection; Abscess; Osteomyelitis; Septic arthritis; Intravenous drug abuse
Introduction
Extremity infections in Intravenous Drug Abusers (IVDA) can be due localised reaction at the injection site or due to haematogenous spread. Emergency, surgical and orthopaedic clinicians have noticed an increase in the incidence of soft tissue abscess, osteomyelitis and septic arthritis presentations in past decade with a change in the microbiology on culture. Initial literature suggested Pseudomonas species as the most common organism [1,2] with Staphylococcus aureusemerging as the most common organism three decades ago. Recent reports have identified oxacillin-resistant Staphylococcus aureus is becoming increasingly common. In the last decade, there was an outbreak of Anthrax in IVDA, with Scotland being at the epicenter. An understanding of infection process and change in microbiology is essential for proper management.
Methods and Materials
A literature search was performed on PubMed to list articles published in last 50 years. MeSH terms infection, abscess, osteomyelitis, drug abuse, intravenous were used. Clinical trials, retrospective studies, review articles and case reports were included to cover all the published work in English literature. Google scholar search was performed to look at current epidemiology and prevalence of IVDA in United Kingdom. The following discussion will address the current prevalence, common presentations, generic management, and change in microbiology of skin abscesses and osteomyelitis in greater detail and will emphasise the importance of these health risks for patients.
Prevalence of the problem
A recent report on the prevalence of IVDA estimated that in 2014 there were 281,000 users in England and more than 50,000 in Scotland, accounting for the largest numbers in Europe [3].
One-third of cutaneous abscesses seen in community and hospital setting are secondary to the complication of intravenous drug abuse [4]. In communities where needle exchange programs are in place, active abscess and chronic wound problem were present in 35% of IVDA [5].
Presentation and management
In patients who receive intravenous drugs for therapeutic reasons, simple localized reaction progressing to mild cellulitis is usually self-limiting and rarely results in abscess formation. However, unsterilized needles, multiple attempts to inject in already thrombosed veins, subcutaneous injections and using intramuscular injections are the main reasons why abscesses and chronic skin wounds are prevalent in IVDA [6].
There is often delay in presentation to the hospital unless there is systematic involvement. Most common sites for abscesses are forearm, cubital fossa, dorsum of the hand, groin, thighs and feet [7]. A high index of suspicion and requesting a plain radiograph of the involved area can show broken needles in soft tissues that can be responsible for delayed healing and chronicity of the abscesses. Pseudo aneurysm of brachial and femoral arteries should be suspected when an IVDA presents with an abscess over cubital and groin region respectively. An ultrasound scan is useful investigations to not only confirm the size of the collection but also to alarm the surgeon before incision and drainage is performed. Routine blood tests usually show only mild abnormality of raised WBC, ESR or CRP. A blood culture can be positive if there is bacteraemia. Wound swabs and tissue for culture are the most important investigation to provide treatment with appropriate antibiotics. Early consult with microbiologist and local guidelines for the antibiotic regime is of utmost importance [8].
Acute haematogenous spread can result in osteomyelitis, and chronic discharging sinuses can cause septic arthritis of the underlying joint (elbow in the case of cubital fossa abscess and hip joint in cases with groin abscess), but fortunately bone and joints infection are much less common in this population. Magnetic resonance imaging is the investigation of choice for confirming bone involvement [9]. A prolonged course of antibiotic is necessary. However, sub-optimal empirical antibiotic treatment in absence of culture result and noncompliance remain two main reasons behind the emergence of antibiotic resistance [10].
Microbiology
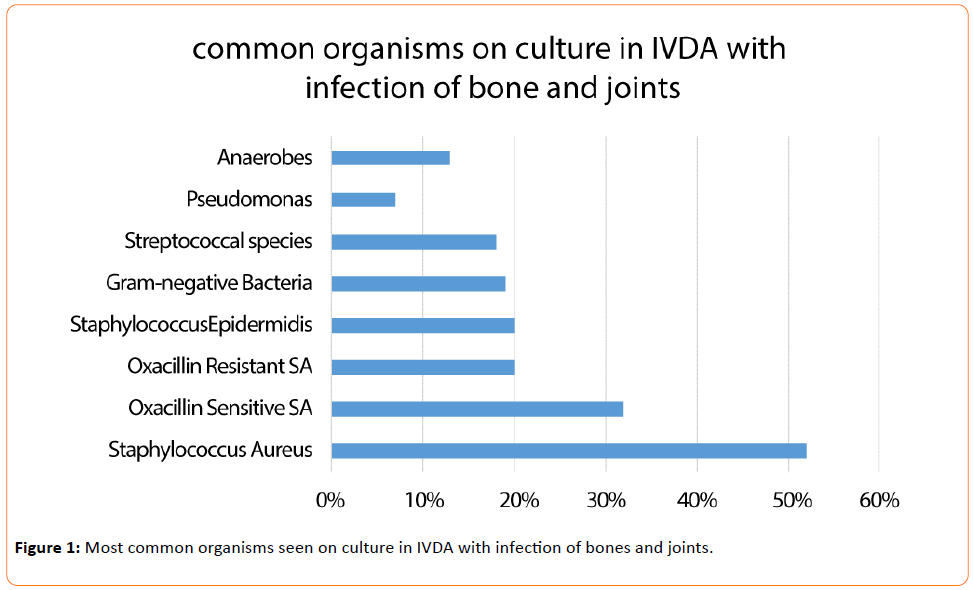
For intravenous drug users, there are significant risks of bone and joint infections, particularly in the tissue areas that surround injection sites. Most common pathogens isolated by culture in these infections are given in Figure 1. Four decades ago estimated the number of IVDA was 5000 in England [3], there were just a few reports on soft tissue complications in IVDA, and most common pathogen reported then was Pseudomonas. Since then there have been emerging evidence on the prevalence of several other organisms. In a study involving over 200 patients, 52% cases were attributed to Staphylococcus aureus, while Staphylococcus epidermidis was a contributing factor in 20% of cases; furthermore, in 20% (44) of these infections, there was no growth when cultures were taken [8]. Change in microbiology from Pseudomonas species to Staphylococcus species is due to the change in the way drug is diluted. In early 1970's pentazocine was mixed with tap water, a source of Pseudomonas aeruginosa but since 1980's heroin diluted with boiled water (which kills gram negative organisms) became the most commonly used substance for abuse [11].
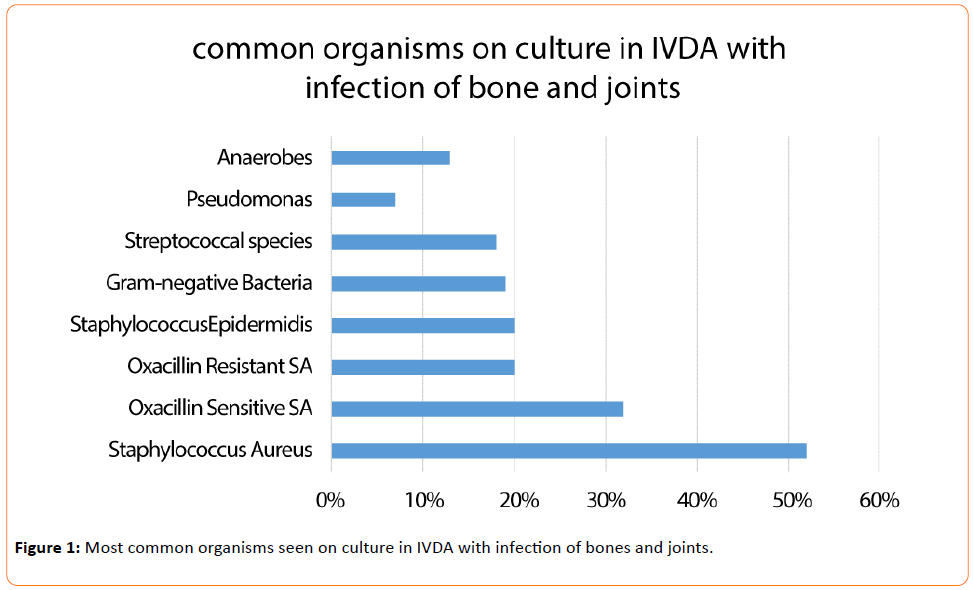
Figure 1: Most common organisms seen on culture in IVDA with infection of bones and joints.
For patients with osteomyelitis, polymicrobial infections were a contributing factor, along with Gram-negative organisms and anaerobic infections in patients [10]. Therefore, it is important to identify antibiotic therapies that will be effective for treatment, but to exercise caution when addressing the risks related to these therapies due to possible resistance.
Another cross-sectional study was conducted with the Baltimore City Needle Exchange Program (BNEP) for persons with abscesses and chronic wounds, evaluating skin care methods and injection practices; of the 152 participants involved in the study, around 34% had either chronic wound or an abscess [5,6].
Intravenous drug use also poses an increased risk of soft tissue infections in the upper extremities and in a retrospective study of 855 patients, who were IVDA, 359 patients of the 694 who tested positive for organisms presented with S. aureus [10]. Furthermore, it was evident that many of these patients were resistant to oxacillin, with an 82% rate of resistance in 2005; other infections were caused by microaerophilic streptococci in 37% of the identified cases. To treat these infections appropriately, authors recommended broad-spectrum antibiotic therapies. One randomized control trial looked at the efficacy of ampicillin/sulbactam and cefoxitin in the treatment of abscess, and both were very efficient in eradicating pathogens [12]. The most common organism was streptococcal species which was found to be in 37% of abscesses in IVDA.
Inappropriate antibiotic use such as overly broad agents, incorrect drug dosing or duration, and poor drug adherence, is a contributing factor to the problem of drug resistance in this group. For some patients, there is a delay in seeking treatment for an infection due to lack of knowledge of the severity of the infection, and furthermore, the use of heroin, which serves as an analgesic to mask the pain associated with these infections, may also be a causative factor in delaying evaluation and treatment. There are also concerns associated with wait times within emergency rooms or physician offices, which may lead to other measures that are less safe and hygienic for patients.
A study in Scotland, United Kingdom reported on more than 100 patients who were suspected to have developed Bacillus anthracis infection (47 culture positive) following use of contaminated heroin. Usual presentation was development of induration and discoloration at injection site with or without abscess formation. Unfortunately, the mortality rate for this type of infection is very high, given the severe nature of the bacteria and its rapid influence on organs and systems [13,14].
Recent Anthrax outbreak created initial difficulty in diagnosis due to atypical presentation (absence of eschar), and most of the early cases were treated with a combination of several different antibiotics in the absence of a correct diagnosis [13-15].
One of the most common dreaded infections associated with intravenous drug abuse is Methicillin-Resistance S. aureus (MRSA), which is a serious skin infection with a complex treatment regimen due to significant antibiotic resistance. There is a very high percentage of IVDA with the colonization of MRSA and is associated with infections in more than 50% of the colonised-IVDA [14]. High-risk behavior such as sharing unsterilized needles and physical contact is responsible for transmission within IVDA community. These IVDA who are colonised with Community-Acquired MRSA (CA-MRSA) then act as a source in the community. To effectively eradicate CAMRSA transmission, appropriate treatment of skin and soft tissue infection is necessary [16,17]. Surveillance programs should be in place to address the nature of these infections more closely and to address treatment alternatives.
For intravenous drug users, it is necessary to evaluate the risk factors that are associated with this practice and the skin infections that may result; therefore, it is necessary to determine the best possible approach in order to ensure that these risk factors are minimized among this population group [18]. Some of the most common risk factors include sharing needles for injection purposes, along with skin cleansing behaviors that are either limited or are nonexistent; therefore, these practices must be addressed in the context of promoting prevention and in recognizing the risks associated with intravenous drug use. With the potentially high risk of developing skin infections and abscesses in response to intravenous drug use, recognizing the potential severity of infection must serve as a viable educational tool to improve the response rate.
Osteomyelitis and Septic arthritis in adjacent joint or uncommonly in remote joint are difficult to manage due to late presentations, polymicrobial nature of the infection and also because a high number of patients do not follow treatment advice. Nearly half of the patients with osteomyelitis will have a polymicrobial infection which is not the case in septic arthritis (only 15% are polymicrobial). Organisms from skin flora, sharing unsterile needle and substance carrying organism are possibly responsible for this polymicrobial infection. Available evidence suggests that MRSA is the most common pathogen responsible for septic arthritis in IVDA. In a retrospective cohort study of 58 IVDA patients who had osteomyelitis/septic arthritis, Staphylococcus species was the most common organism, along with secondary causes that include Streptococcus, Pseudomonas, and Serratia. MRSA infections were most commonly identified in the hip joint (57.1%), while Methicillin-Sensitive Staphylococcus aureus (MSSA) infections were most commonly identified in the knee joint (94.4%) [15]. This finding can be explained by groin being common injection site, is subjected to repeat injections, thrombosis, abscess formation and ultimately septic arthritis of the native hip joint. Empirical antibiotic treatment for septic arthritis in IVDA should be vancomycin or linezolid due to the high prevalence of MRSA in this group [19].
Conclusion
Management of infection as a result of intravenous drug abuse is challenging, careful evaluation of causative organism and microbiologist’s advice is important to avoid development of antibiotic resistance. A multidisciplinary team approach for prevention is critically important. It is evident that some types of infections are caused by bacteria that are highly resistant to antibiotic therapies, including those related to ORSA and MRSA; therefore, healthcare providers must address the problem and should promote preventive strategies. To avoid development of antibiotic resistance, the administration of antibiotics must be supported by a framework that includes a comprehensive education and treatment strategy.
9054
References
- Gifford DB, Patzakis M, Ivler D, Swezey RL (1975) Septic arthritis due to Pseudomonasin heroin addicts. JBJS 57:631-635.
- Kido D, Bryan D, Halpern M (1973)Haematogenous osteomyelitis in drug addicts. Am J Roentgenol Radium TherNucl Med 118:356-363.
- Peter Reuter, Alex Stevens (2007) An Analysis of UK Drug Policy, A Monograph Prepared for the UK Drug: Policy Commission.
- Jenkins TC, Knepper BC, Jason Moore S, Saveli CC, Pawlowski SW, et al. (2015)Microbiology and initial antibiotic therapy for injection drug users and non-injection drug users with cutaneous abscesses in the era of community-associated methicillin-resistant Staphylococcus aureus. AcadEmerg Med22:993-997.
- Smith ME, Robinowitz N, Chaulk P, Johnson KE (2015)High rates of abscesses and chronic wounds in community-recruited injection drug users and associated risk factors.J Addict Med 9:87-93.
- Giudice PD (2004) Cutaneous complications of intravenous drug abuse. Br J Dermatol150: 1-10.
- Fink DS, Lindsay SP, Slymen DJ, Kral AH, Bluthenthal RN (2013) Abscess and self-treatment among injection drug users at four California syringe exchanges and their surrounding communities.Subst Use Misuse 48:523-531.
- Allison DC, Miller T, Holtom P, Patzakis MJ, Zalavras CG (2007) Microbiology of upper extremity soft tissue abscesses in injecting drug abusers. Clinical orthopaedics and related research 9-13.
- Alcantara AL, Tucker RB, McCarroll KA (2002) Radiologic study of injection drug usecomplications.Infect Dis Clin North Am16:713-743.
- Allison DC, Holtom PD, Patzakis MJ, Zalavras CG (2010) Microbiology of bone and joint infections in injecting drug abusers. ClinOrthopRelat Res468:2107–2112.
- Berger T, Kassirer M, Aran AA (2014)Injectional anthrax - New presentation of an old disease. Eurosurveillance 19.
- Knox D, Murray G, Millar M, Hamilton D, Connor M, et al. (2011) Subcutaneous anthrax in three intravenous drug users: a new clinical diagnosis. JBJS Br 93: 414-417.
- Russell, Pedersen L, Jensen M, Søes AV, Marie V, et al. (2013) Two anthrax cases with soft tissue infection, severe oedema and sepsis in Danish heroin users. BMC infectious diseases 13.
- El-Shariff A, Ashour HM (2008) Community-acquired methicillin-resistant Staphylococcus aureus(CA-MRSA) colonization and infection in intravenous and inhalational opiate drug abusers. ExpBiol Med (Maywood) 233:874-880.
- Hsin H, Cohen SH, King JH, Monchaud C, Nguyen H, et al. (2008) Injecting drug use and community-associated methicillin-resistant Staphylococcus aureusinfection. DiagnMicrobiol Infect Dis 60: 347-350.
- Maloney S, Keenan E, Geoghegan (2010) What are the risk factors for soft tissue abscess development among injecting drug users? Nursing Times 106: 21-24.
- Peterson TC, Claire P, Zekaj M, Hudson I, Fakhouri G, et al. (2014) Septic arthritis in intravenous drug abusers: a historical comparison of habits and pathogens. The Journal of emergency medicine 47: 723-728.
- Talan DA, Summanen PH, Finegold SM (2000) Ampicillin/sulbactam and cefoxitin in the treatment of cutaneous and other soft-tissue abscesses in patients with or without histories of injection drug abuse.Clin Infect Dis31:464-471.
- Shirtliff ME, Mader JT (2002) Acute septic arthritis. ClinMicrobiol Rev 15:527-544.