Keywords
Colonoscopy; Diagnostic yield; Port Harcourt; Nigeria
Introduction
Colonoscopy became increasingly popular from seventies of the last millennium [1]. With advancements in optics, imaging modalities, mechanics, techniques, and instrumentation it has become the procedure of choice for evaluation of lower gastrointestinal bleeding, colorectal cancer (CRC) screening, and polyp surveillance.2-5It allows for complete mural examination and management of diseases in the anus, rectum, colon, and terminal ileum. This procedure is cost effective as it can be used to obtain tissue (biopsy) and perform interventional procedures like total resection of lesion, haemostasis, dilatation etc.
An adequate knowledge of normal anatomy and its variants is central to the appreciation of pathological changes or abnormalities during colonoscopy. These pathologies include polyps, diverticula and tumours among other findings. A critical threshold standard is needed to ensure patient safety and successful colonoscopy. Some of these are gentle, minimal blind pushing, keeping the lumen within view, periodic and frequent withdrawal motions for straightening, and avoidance of mucosal whitening or reddening (“red out”) by scraping or sliding by the wall of the colon [2]. Pain and incomplete colonoscopy are generally due to poor bowel preparation, loop or bowing formation and resultant mesenteric stretching.
Recent advancements in magnetic imaging have been helpful in facilitating colonoscopy by detecting looping and facilitating straightening and shortening maneuvers [3]. The utilization of good basic technique and an appreciation and application of standardized approach to difficult intubation (redundancy, difficult sigmoid, poor tolerance to sedation) help to yield improved maneuverability and successful colonoscopy [4]. Colonoscopy is yet to become routine in many developing countries as there are few endoscopy facilities and trained personnel. This study is the first prospective study on colonoscopy from Port Harcourt a metropolis in Nigeria- a populous African country.
This study aims to assess the diagnostic yield of colonoscopy from a city in Niger –Delta region of Nigeria.
Patients and Methods
Study setting
This study was conducted in a referral endoscopy facility in Port Harcourt in Niger Delta region of Nigeria from March 2014 to October 2017.
Study design
This is a prospective study of all consecutive patients referred for colonoscopy. A proforma was used to record demographics, indication for procedure, location, type of lesion found by colonoscopy and the pathologic diagnosis. The diagnostic yield of procedure was defined by the detection of pathology including incidental findings. Relevant approval was obtained from the Ethical committee of the establishment. An informed consent was also obtained from patient or guardian for minors according to Helsinki declaration 1975.
Pre-procedure preparation
All patients had a 2-day dietary restriction to fluids/fluid diet preceding morning of procedure. There was prior bowel cleansing using polyethylene glycol PEG 3350 or Sodium picosulphate/citrate or combination of bisacodyl and castor oil based on availability of stock. Conscious sedation with intravenous Benzodiazepine (diazepam 2.5-5 mg) and pentazocine 30mg was administered to all patients before procedure. The endoscopy equipment used was Karl Storz (Germany) video-colonoscope 13925PKS light source/pump and camera control unit.
Procedure
All the procedures were performed by the same endoscopist (ERO). The colonoscope was inserted after a digital rectal examination with patient in left lateral position. A change to supine, right lateral or prone position was occasionally done as needed. The patients were observed for a minimum of 30 minutes before discharge. They were counseled to resume normal diet and call to report any complications.
Statistical analysis
The data was inputted into Statistical Package for Social Sciences, INM SPSS for Windows and Version 20.0 (Armonk, NY: IBM Corp). The continuous variables are presented as mean ± standard deviation (SD) and categorical variables as percentages. These variables were further analyzed by Chisquare and Fisher’s exact test appropriate for statistical significance of observed differences for categorical variables.
Results
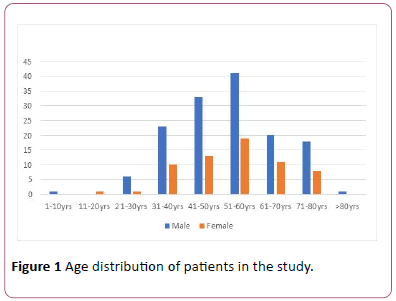
During the study period 212 colonoscopies were performed in 210 patients. The age range of studied patients was from 4 rears to 86 years (Figure 1); the mean age was 53.5 ±13.9 years. There were 148 males and 64 females; M: F ratio of 2.3:1. Patients in the 6th decade of life had the highest frequency of procedures.
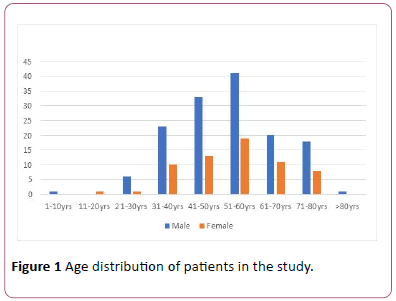
Figure 1: Age distribution of patients in the study.
The leading indications for colonoscopy were bleeding per rectum 119 (55.9%), lower abdominal pains 30 (14.1%) and change in bowel habit 27 (12.7%), screening 10 (4.7%), positive faecal occult blood test 6 (2.8%) (Table 1).
| Indication |
Number |
Diagnostic yield |
Percentage |
| Bleeding per rectum |
119 |
109 |
51.40% |
| Lower abdominal pain |
30 |
16 |
7.50% |
| Change in bowel habit |
27 |
17 |
8.00% |
| Surveillance |
2 |
0 |
0% |
| Screening |
10 |
1 |
0.30% |
| Unexplained anaemia |
2 |
2 |
0.90% |
| Positive faecal occult blood test |
6 |
6 |
2.80% |
| Tenesmus |
2 |
2 |
0.90% |
| Flatulence |
3 |
1 |
0.50% |
| Others |
11 |
4 |
1.90% |
| Total |
212 |
159 |
75.00% |
Table 1: Relationship between indication and diagnostic yield of colonoscopy.
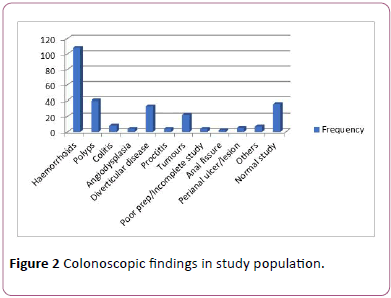
The pathologies seen included: haemorrhoids 121 (57.1%); polyps 38 (17.9%); diverticulosis/diverticular disease 31 (14.6%), and colorectal tumour 20 (9.4%). A normal study was recorded in 36 (17.0%) cases thus giving a diagnostic yield of 83.0%. The colonoscopic finding was related to primary indication in 159 (75%) (Table 1). Pathologies seen in 20 (9.4%) cases were unrelated to the primary indication for colonoscopy (incidental findings). Seventy-four cases (34.7%) had multiple pathologies with more than 4 pathologies in different sites seen in 18 cases (8.5%).
The anus and anal cane the most common sites involved 128 (41.3%), others were recto-sigmoid 76 (24.7%) and transverse colon 44 (14.2%) (Table 2). The pathologies seen are as shown in Figure 2.
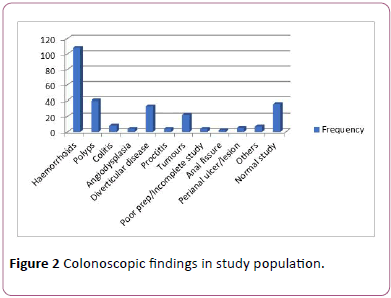
Figure 2: Colonoscopic findings in study population.
| Location of lesion |
Frequency |
Percentage (%) |
| Anal canal and anus |
128 |
41.3 |
| Rectum |
43 |
13.9 |
| Sigmoid colon |
33 |
10.8 |
| Descending colon |
26 |
8.4 |
| Transverse colon |
44 |
14.2 |
| Ascending colon |
32 |
10.3 |
| Caecum |
4 |
1.3 |
| Total |
310 |
100 |
Table 2: Site distribution of lesions.
Histopathologic diagnosis from 67 biopsies taken is as shown in Table 3. Chronic non-specific colitis was the leading histopathologic diagnosis -20 (29.9%). The biopsy of detected polyps in this study revealed more than half of these histologically reported as inflammatory polyps.
| Histopathology |
Frequency (%) |
| Unremarkable mucosa |
1 (1.5) |
| Polyps |
| Inflammatory |
16 (23.9) |
| Hyperplastic |
4 (6.0) |
| Adenomatous |
11 (16.4) |
| Inflammatory disease |
| Non-specific colitis |
20 (29.9) |
| Ulcerative colitis |
1 (1.5) |
| Radiation proctitis |
1 (1.5) |
| Colorectal tumour |
| Adenocarcinoma |
12 (17.9) |
| Non-Hodgkins lymphoma |
1 (1.5) |
| Total |
67 (100) |
Table 3: Histopathologic diagnosis of cases.
Discussion
Colonoscopy has emerged as the procedure of choice for evaluation of lower gastrointestinal bleeding, colorectal cancer (CRC) screening, and polyp surveillance with its ability to allow for therapeutic intervention [5-7]. In this study a high diagnostic yield of 83% was recorded for this endoscopic procedure as no abnormality was observed in 36 cases (17.0%). These negative results were as valuable as the positive observations as it provided relief to both the patient and the managing physician [8]. Some studies from different parts of Nigeria have reported diagnostic yield between 70% to 80% [9,10]. In Egypt and Iran, reports of 72% and 65% diagnostic yield respectively have been recorded for colonoscopy [11,12]. Across Europe, significant pathologies (cancer, adenomatous polyps, angiodysplasia, and new diagnoses of inflammatory bowel disease) is reported in 25% of colonoscopies [13]. There is a significantly greater rate of neoplasia detection during colonoscopy with time dependent withdrawal [14]. A careful examination with minimum withdrawal time of at least 8 minutes after the endoscope has been navigated to the caecum was adopted in this study increasing the chance of pathology detection. In addition, only few centers are providing endoscopic services in the city where the study was undertaken as such only patients with established diseases are likely to present for the procedure.
The fourth, fifth and sixth decades of life were the most frequent age groups of patients in increasing order of frequency with a male predominance. In a multi-centre colonoscopy study in another metropolitan city in Nigeria, the fourth decade of life followed by the fifth were the most frequent age of patients and a male predominance was similarly reported [10]. Owing to lack of adequate facilities and expertise for colonoscopy service in Africa patient selection according to diagnostic yield has been suggested against open access [15]. From our findings, colonoscopy is strongly recommended in middle- aged patients with symptomatic colonic pathologies. The five major indications for colonoscopy were rectal bleeding, change in bowel habit, abdominal pain, positive faecal occult blood test and routine screening. The anus and anal canal had the most frequent pathology - haemorrhoids (Table 2). Next, is the rectosigmoid area which had over one fifth of the pathologies recorded. This trend is like findings in a study from the UK which showed a high correlation of colonoscopy pathology site with surgery findings [16].
The most common pathologies seen in decreasing order of frequency were haemorrhoids, polyps, diverticular disease and colon cancer. Multiple pathologies were a significant observation in almost one quarter of the study population. In a similar study from Ghana, the three most common pathologies recorded were haemorrhoids, tumours and proctocolitis (32.3%, 9.0% and 4.2% respectively) [17]. A single case of ulcerative colitis was recorded during the study period and no case of Crohn’s disease was seen. This confirms that inflammatory bowel disease IBD is still rare in Nigeria with few reports of sporadic cases [18,19]. However, in Nile Delta, Egypt, IBD has been reported in 25% of cases, haemorrhoids 18% and diverticulosis 2% [11]. Surprisingly, diverticular disease, which is more common to western population attributable to a low residue diet pattern, was the 3rd leading pathology recorded in our metropolitan study. Results of similar studies confirm a shift in the epidemiology of this disease in Africa [9,10,20]. It is note-worthy that no case with clinical suspicion or endoscopic diagnosis of ischaemic colitis was observed in this study.
A limitation of this study is the non-assessment of sensitivity or specificity of colonoscopy as further complimentary investigations was not evaluated. Also, there was a high rate of more than 72-hour delay in the presentation of the referred cases with bleeding per rectum which may lower the diagnostic yield in these delayed cases. Although, colonoscopy is generally safe, it is an invasive procedure that can rarely be complicated by perforation, hemorrhage and infection [21,22]. None of these complications was recorded in this study. There is the need for the relevant expertise and meticulous safety measures to be undertaken in this invaluable diagnostic and therapeutic modality for colonic pathologies.
Conclusion
Colonoscopy is a very useful investigation for the lower digestive tract with a high diagnostic yield in patients with lower gastro-intestinal symptoms especially in the middle- age population. There is an observed shift in epidemiology of diverticular disease in this subset of Sub-Saharan African population studied.
References
- Wolff WI, Shinya H, Geffen A, Ozaktay SZ (1972) Colonofiberoscopy: A new and valuable diagnostic modality. Am J Surg 123: 180-184.
- Landmann RG, Francone TD (2017) Anatomic basis of colonoscopy. In: Lee S, Ross H, Rivadeneira D, Steele S, Feingold D (eds) Advanced Colonoscopy and Endoluminal Surgery. Springer, Cham.
- Wehrmann K, Frihmorgen P (2002) Evaluation of a new three-dimensional magnetic imaging system for use during colonoscopy. Endoscopy 34: 905-908.
- Rex DK, Chen SC, Overhiser AJ (2007) Colonoscopy technique in consecutive patients referred for prior incomplete colonoscopy. Clin Gastroenterol Hepatol 5: 879-883.
- US Preventive Services Task Force (2000) Colon cancer screening (USPSTF recommendation). J Am Geriatr Soc 48: 333-335.
- Rex DK, Helbig CC (2007) High yields of small and flat adenomas with high-definition colonoscopes using either white light or narrow band imaging. Gastroenterology 133: 42-47.
- Henley SJ, King JB, German RR, Richardson LC, Plescia M, et al. (2010) Surveillance of screening detected cancers (colon and rectum, breast, and cervix)—United States, 2004-2006. MMWR Surveill Summ 59: 1-25.
- Thiis-Evensen E, Seip B, Vatn MH, Hoff GS (2006) Impact of a colonoscopic screening examination for colorectal cancer on later utilization of distal GI endoscopies. Gastrointest Endosc 64: 948-954.
- Akere A, Oke TO, Otegbayo AO (2016) Colonoscopy at a tertiary healthcare facility in Southwest Nigeria: Spectrum of indications and colonic abnormalities. Ann Afr Med 15: 109-113.
- Onyekwere CA, Odiagah JN, Ogunleye OO, Chibututu C, Lesi OA (2013) Colonoscopy practice in Lagos, Nigeria: A report of an audit. Diagn Ther Endosc 2013: 798651.
- El-Batea H, Enaba M, El-Kassas G, El-Kalla F, Elfert AA (2011) Indications and outcome of colonoscopy in the Middle of Nile Delta of Egypt. Dig Dis Sci 56: 2120-2123.
- Joukar F, Majd SK, Fani A, Nazari N, Mansour-Ghanaei F (2012) Colonoscopy outcome in North of Iran (Guilan):2006-2009. Int J ClinExp Med 5: 321-325.
- Gonvers JJ, Harris JK, Wietlisbach V, Froehlich F (2006) A European view of diagnostic yield and appropriateness of colonoscopy. Hepato-gastroenterology 54: 729-735 .
- Barclay RL, Vicari JJ, Greenlaw RL (2008) Effect of a time-dependent colonoscopic withdrawal protocol on adenoma detection during screening colonoscopy. Clin Gastroenterol Hepatol 6: 1091-1098.
- Berkowitz I, Kaplan M (1993) Indications for colonoscopy: An analysis based on indications and diagnostic yield. SAMJ 83: 245-248.
- Moug SJ, Fountas S, Johnstone MS, Bryce AS, Renwick A, et al. (2017) Analysis of lesion localisation at colonoscopy: Outcomes from a multi-centre U.K. study. Surg Endosc 31: 2959-2967.
- Dakubo JCB, Seshie B, Ankrah LNA (2014) Utilisation and diagnostic yield of large bowel endoscopy at Korle Bu Teaching Hospital. J Med Biomedical Sci 3: 6-13.
- Alatise OI, Otegbayo JA, Nwosu MN, Lawal OO, Ola SO, et al. (2012) Characteristics of inflammatory bowel disease in three tertiary health centers in Southern Nigeria. WAJM 31: 28-33.
- Ukwenya AY, Ahmed A, Odigie VI, Mohammed A (2011) Inflammatory bowel disease in Nigerians: Still a rare diagnosis. Ann Afr Med 10: 175-179.
- Olokoba AB, Obateru OA, Bojuwoye MO, Olatoke SA, Bolarinwa OA, et al. (2013) Indications and findings at colonoscopy in Ilorin, Nigeria. Niger Med J 54: 111-114.
- Arora G, Mannalithara A, Singh G, Gerson LB, Triadafilo-Poulos G (2009) Risk of perforation from a colonoscopy in adults: A large population-based study. Gastrointest Endosc 69: 654-664.
- Dominitz JA, Eisen GM, Baron TH, Goldstein JL, Hirota WK, et al. (2003) Complications of colonoscopy. Gastrointestinal endoscopy 57: 441-445.