Keywords
Postsurgical seroma; Incisional hernia; Distal
paravertebral anesthesia (DPVA); Laparotomy;
Hematological parameters
Introduction
Laparotomy is universally designated for exploratory drives
when the clinical diagnosis is inexact or for therapeutic surgical
involvement has been made [1]. It is solitary of the furthermost
conjoint surgical procedures in livestock practice which is
customarily accomplished on standing cattle [2]. However, no
document recorded in standing goats. In Bangladesh a lot of
vegetables (e.g., carrot, radish, cabbage, potato etc.) and cereal
crops (e.g., rice, wheat, pulses etc.) are produced frequently.
When the prices of these products get down in the market and
sometimes excess feeding of the products can create acidosis
with bloat and choke. That time it needs to remove the
materials from rumen with laparotomic intervention. For
Chittagong with a lot of goats in number from the aesthetic
point of view as well as in Hindu religious festival named
Manasha puja, people sacrifice goats for the Goddes Manasha.
So, the laparotomy is common for the above-mentioned
conditions. For research, Shahedul Alam Quaderi Teaching
Veterinary Hospital (SAQTVH) is renowned in Bangladesh and of
courses in the world. We did the intervention as research. In
contrast to general anesthesia, there is less to cardiovascular
depression and no inhibition of the visceral organs in local and
regional anesthesia. During local anesthesia exertion and charge
for the surgery is lower than in general anesthesia [3]. For the
laparotomy, it is an absolute absence of pain in the incision and
occlusion of the abdominal cavity. The mode of action of local
anesthetics comprises blockade of sodium channels, which
checks nerve depolarization. Lidocaine may use by perineural
infiltration, intra-articular or epidural injection provides
excellent analgesia. Lidocaine is the commonly used local
anesthetics in veterinary medicine, but it has a historical
reputation of being toxic to goat kids [4,5]. For the enough
desensitization of the flank, 13th thoracic spinal nerve and the first two lumbar spinal nerves need to be anesthetized.
Elimination of the sensitivity of peritoneum is caused by the
switching of the second lumbar spinal nerve reached. This one
gives a branch that runs on the surface of the peritoneum [6]. In
the literature, there are different methods of local anesthesia for
the laparotomy in the area of hunger pit [3]. The flank area is
easily desensitized by performing a line block, which is the most
commonly used method in food animals [3]. Disadvantages of
this technique are the large volume of local anesthetic and the
lack of relaxation of the back and abdominal muscles [7].
Furthermore, incomplete anesthesia of the deeper layers in
heavy animals as well as hematomas and seromas due to
injections [8]. The infiltration of cutting line with a local
anesthetic may cause tissue damage and wound healing
disorders [9] especially at the addition of vasoconstrictors.
Another disadvantage of line infiltration is an intraoperative
necessary magnification at post-anesthesia that renewed access
waiting until the onset of action is required [7]. Distal
paravertebral anesthesia (DPVA) is intended to be safely in being
pain-free and easy, fast and with little local anesthetic can be
performed [10]. The performance area is complete and uniform
in all layers anesthetized [7]. In inflammatory reactions around
the incision line in the flank or in a relaparotomy with distal
paravertebral anesthesia is better than incision infiltration [3].
The disadvantage of this technique has difficulty in fatty animals.
On the other hand, the orientation leads to anatomical
distinctive points not always safe anesthesia, because the spinal
nerves follow a variable path [6]. One of the dangers of DPVA is
the possibility of penetration of large blood vessels. Besides, it is
the uncertainty of the pelvic limbs upon diffusion of the local
anesthetic in the route of motor nerves [3,7].
Materials and Methods
Study period
The present study was conducted during the period of July
2017 to June 2018 at Shahidul Alam Quadery Teaching
Veterinary Hospital (SAQTVH), Chittagong Veterinary and Animal
Sciences University (CVASU) Chittagong, Bangladesh.
Study area
The study was driven at SAQTVH in Chittagong Veterinary and
Animal Sciences University as case registered and outpatients of
Chittagong Metropolitan area of Chittagong (Figure 1).
Figure 1: Geographical location of study area.
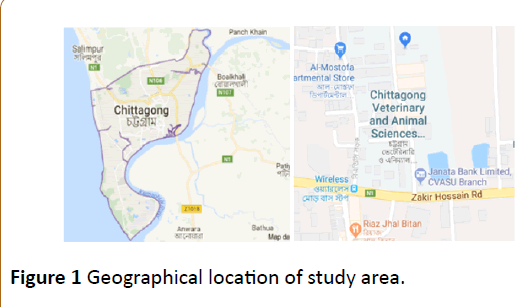
Study design
A total of ten (n=10) samples from two groups mixed with
male and female (5 male and 5 female of local breed) of
different ages were chosen for this study (Figure 2).
Figure 2: The overall experimental design of this study.
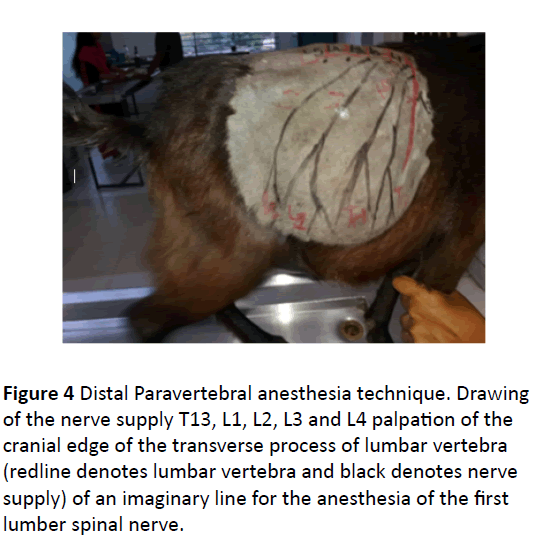
Preoperative measures
For laparotomy, the goats were in a stationary or a fixed
mobile togetherness before the start of blocking, proper shaving
from T13 to L4 and sketch diagram of nerve supply for proper
nerve block was drawn for proper detection and identified the
nerves for proper anesthesia and pain sensation measure.
Anesthesia
As a local anesthetic, lidocaine 2% solution came without
further additives for use (Jasocane 2%, Jayson pharma Dhaka
Bangladesh) Lidocaine does @6 mg/kg BW [11] for two types of
techniques applied as distal paravertebral anesthesia and
modified line infiltration. After setting the respective anesthesia
was waited at least for 5 minutes, before the operation started
[2].
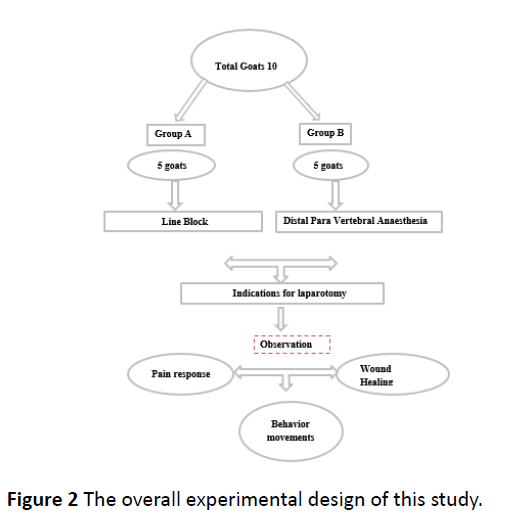
Surgical procedure
Feed and water were withdrawn from animals at least 12
hours prior to the surgery. The left flank region of each goat in
both groups was prepared for routine aseptic surgery by clipping
the hairs around the proposed surgical site; the site was
scrubbed with Povin vet solution containing 10% povidoneiodine
(Opsonin Pharma Limited, Dhaka) and then flushed with
70% alcohol. Regional anesthesia was achieved with a plain 2%
lidocaine hydrochloride and injection (Jason Caine, Jayson
pharma limited, Dhaka).
Goats of both groups were placed on the right lateral
recumbency exposing the left flank. Laparotomy was done
according to the standard procedure described by Ames et al. [11,13,14]. The laparotomy was routinely closed from within
outward; muscle layers were closed using Jonson chromic catgut
of the size of 1/0 and atraumatic ½ circle taper point needle
(Anhui Kangning Industrial Groups, China) using simple
continuous to peritoneum and ford interlock in the muscle layer
(Figure 3).
Figure 3: Surgical procedure.
The subcutaneous layer was closed using Jonson chromic
catgut of the size of 2/0 and atraumatic ½ circle taper point
needle using simple continuous suture pattern. The skin was
closed using a vertical mattress suture pattern with nylon of the
size of 0 and atraumatic 3/8 curved, cutting needle (Agary
Pharmaceuticals Ltd, Xinghuai, China). Meloxicam injection at
the rate of 0.5 mg/kg subcutaneous injection (ACME
Pharmaceutical, Dhaka) was administered for 3 days after
surgery to take care of postoperative pain. Ampicillin injection at
the rate of 20 mg/kg BW (ACI Pharmaceutical, Dhaka) was
administered for 5 days after surgery to control the secondary
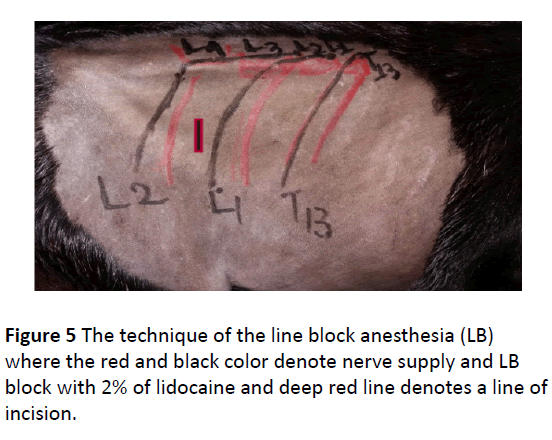
bacterial infection (Figure 5).
Distal paravertebral anesthesia (DPVA)
The skin of the left last ribs to fourth lumber transverse
process was clipped and scrubbed with disinfectant over the
surgical area where the needle was introduced. The distal
paravertebral nerve block desensitizes the dorsal and ventral
rami of the spinal nerves T13, L1, and L2 at the distal ends of the
transverse processes of L1, L2, and L4, respectively. A 23-gauge,
3.5 cm needle was inserted ventral to the transverse process,
and 6 ml of local anesthetic was infused in a fan-shaped pattern
(Figure 4).
Figure 4 Distal Paravertebral anesthesia technique. Drawing
of the nerve supply T13, L1, L2, L3 and L4 palpation of the
cranial edge of the transverse process of lumbar vertebra
(redline denotes lumbar vertebra and black denotes nerve
supply) of an imaginary line for the anesthesia of the first
lumber spinal nerve.
Figure 5 The technique of the line block anesthesia (LB)
where the red and black color denote nerve supply and LB
block with 2% of lidocaine and deep red line denotes a line of
incision.
The needle was removed completely and then reinserted or
redirected dorsal to the transverse process, in a caudal direction,
where 2 ml of local anesthetic was again infused in a fan-shaped
pattern. This procedure was repeated for the transverse
processes of the L2 and L4 lumbar vertebrae of spinal nerves.
Line block (LB)
A 23-gauge 3.5-cm needle is used to infuse multiple small
injections of 6 mL of local anesthetic solution subcutaneously
and into the deep muscle layers and peritoneum. The pain of
successive injections may be alleviated by placing the edge of
the needle into the edge of the previously desensitized area at
an approximately 20-degree angle (Figure 5).
Surgical wound assessment
The clinical appearance of the skin was assessed and scored
twice:18-24 hours and 10-25 days after surgery as described by
Sylvestre et al. [15] using a 4-point scoring scale, based on the
following criteria: discharge, swelling, erythema, and
dehiscence. Mostly complication was seen after surgery to
monitor the wound to know the wound healing conditions.
Hematology
Blood samples were collected from each animal in the groups
through the jugular vein after thorough disinfection of the area
with 70% alcohol, the sample was collected using 5 mL syringe
and needle into EDTA bottles. The samples were collected before
surgery as a baseline (T0), 24 hours after anesthesia (T24) and
one week after surgery (T7). Physiological parameters were
taken manually (heart rate taken by auscultation with a
stethoscope, pulse rate taken by digital counting, respiration by
counting abdominal movement, rectal temperature with a
clinical thermometer) at intervals of 0, 30, 60 minutes and 24
hours after lignocaine administration. The samples were
analyzed using digital hematology analyzer (Full Automated
Blood Cell Counter PCE-210, Erma Inc, Tokyo, Japan) according
to the procedure described [16,17].
Intra- and postoperative complication
Intra and post-surgical complications were assessed using a 3-
point scoring system designed, parameters considered were
intraoperative hemorrhages, postsurgical seroma, incisional
hernia, and wound fistula described by a protocol from
Abubakar et al. [18] (Table 1).
| Outcome |
Scores |
| 0 |
1 |
2 |
| Haemorrhage |
None |
Mild |
Severe |
| Seroma |
None |
Mild |
Severe |
| Wound fistula |
None |
Mild |
Severe |
| Incisional hernia |
None |
Mild |
Severe |
Table 1 Criteria used to score intraoperative and postsurgical complications.
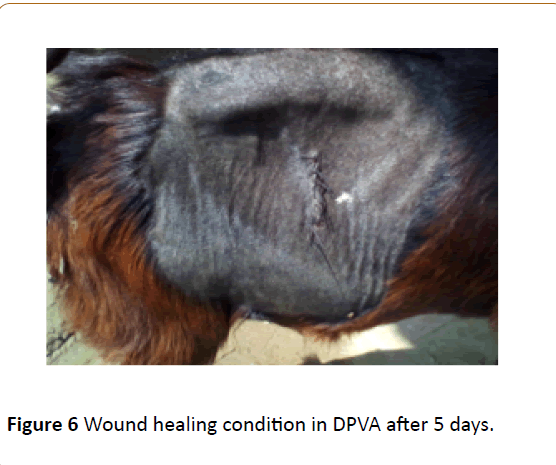
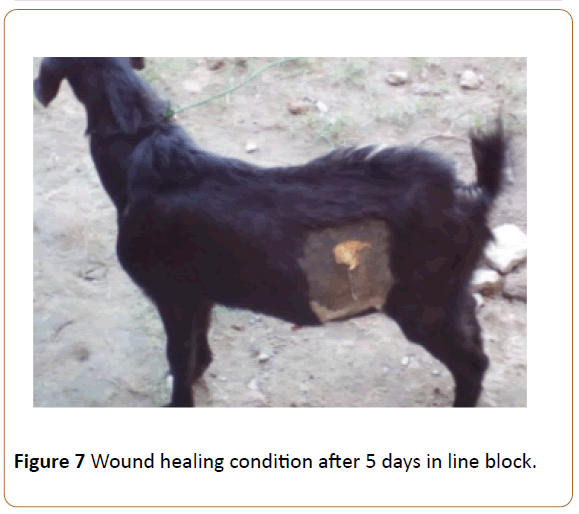
Subjective healing interval
Subjective healing interval was determined by visual
observation and taking notes of days of apparent surgical site
healing b (Figures 6 and 7).
Figure 6 Wound healing condition in DPVA after 5 days.
Figure 7 Wound healing condition after 5 days in line block.
Data collection and analysis
In the anesthesia protocol, the reactions of the animal to the
set the local anesthesia in six given reaction degrees noted
(Table 2). The documentation also included the required amount
of local anesthetic and the time required for the performance of
local anesthesia. In the operation log, there were the pain
reactions in the various stages of the procedure detained (Table
2). In an evaluation of reaction with grade 0 was allowed to the
animal during the carried-out action showed no reaction.
Resulted in a rating with grade 1 to 3, the animal showed
nonspecific reactions that were not in connection with the
manipulations of the anesthetist or the surgeon had to stand, so
no statement regarding allow pain. The animal left clear signs of
restlessness and defense resulted in a rating with the reactions
of grades 4 to 6 considered to be specific. Out of 10 goat
patients, 6 averaged 7 days (Maximum 25 days) daily in the clinic
to be examined. Creating the logs and recording the data were
done after an introduction to the assessment of the BCS, in the
anesthetic methods and in the surgical procedure. For data
entry specially created data sheets were used in the “Microsoft Excel, Windows Version 10”. The statistical evaluation was done
with the “Data Analysis” tools. The differences in the mean
values were calculated by “ t-test. Two samples assuming
unequal variances ” . For comparisons between forms of
anesthesia, the odds ratio (OR) determined. A p-value of <0.05
was considered significant.
| Degree of reaction |
|
Behavior |
| 0 |
Nonspecific reaction
|
No reaction |
| 1 |
Slight skin or muscle twitching (slight Moan) |
| 2 |
Distinct muscle twitching (strong moaning) |
| 3 |
Trippeln / unrest |
| 4 |
Defensive movements like hitting with the leg |
| 5 |
Specific reaction |
Dodge attempts such as going back and forth |
| 6 |
Outbreak attempt / intention to go down |
Table 2 Grading of patient reactions that occurred during the application of lidocaine, during abdominal incision/closure and during exploration of the abdominal cavity.
Table 2 Grading of patient reactions that occurred during the
application of lidocaine, during abdominal incision/closure and
during exploration of the abdominal cavity.
Results
Both the pre-piercing and the subsequent application of the
local anesthetic caused pain reactions. The risk of an animal
showing a pricking response was significantly greater in DPVA
when applying the local anesthetic. Proved at the LB the piercing
and the anesthetic application is the same pain. Regarding the
surgical opening of the abdominal cavity, there were some
significant differences. The average pain score line block
anesthesia was more painful than the average pain score in
distal paravertebral anesthesia technique were pain reduction in
the two techniques.
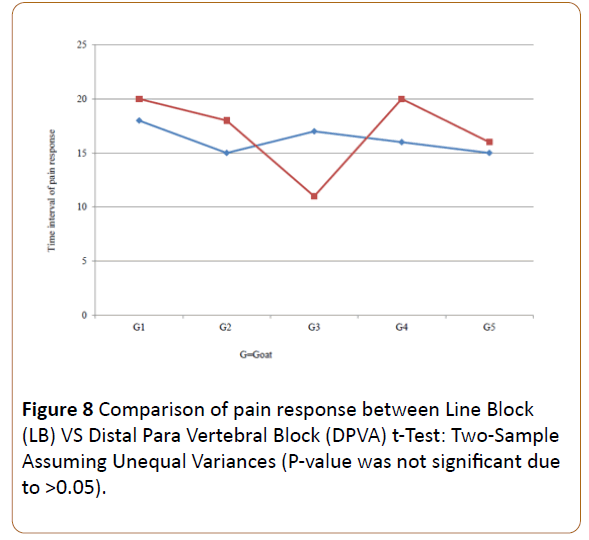
Comparison of pain response between line block (lb)
vs distal para vertebral block (DPVA)
The present study reveals that distal paravertebral anesthesia
is less pain for laparotomy then the Line block anesthesia (Figure
9). The below graph shows the red line as the timing of pain
response in DPVA compared to the timing of pain response in LB
by a blue line. Pain shows a better response in DPVA as less pain
in the specific time of laparotomy (Figure 8).
Figure 8Comparison of pain response between Line Block
(LB) VS Distal Para Vertebral Block (DPVA) t-Test: Two-Sample
Assuming Unequal Variances (P-value was not significant due
to >0.05).
Figure 9Percentage of pain reaction during DPVA and LB for
preparation time and application time (in minutes).
Animals movements behaviors
The present study based on goat movements behaviors which
were my target pain response measurement key for evaluation
and grading. In this study, we can see mostly non-specific
reaction behaviors, so we can say that 2% lidocaine anesthesia
for pain management is good in both interventions. The below
table had taken the responsibility to judge the different
conditions of that two intervention which was necessary for the
study (Table 3).
| Degree of reaction |
|
Behavior |
| 0 |
Nonspecific reaction |
No reaction |
| 1 |
Slight skin or muscle twitching (slight Moan |
| 2 |
Distinct muscle twitching (strong moaning) |
| 3 |
Trippeln / unrest |
Table 3 Grading of patient reactions that occurred during the application of lidocaine during abdominal incision/closure and during exploration of the abdominal cavity.
Table 3 Grading of patient reactions that occurred during the
application of lidocaine during abdominal incision/closure and
during exploration of the abdominal cavity.
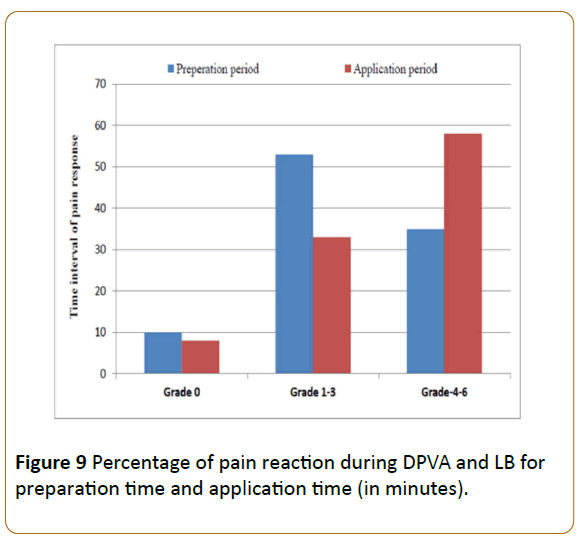
Pain response during time
Pain responses during the preparation time of the patient and
as well as in application time had been separated in three grades
ranges. The bar diagram reveals almost the same pain response
in “grade 0” ranges for both in DPVA and LB. As time advanced,
for the middle bars configured as grade 1-3 got a good knock in
application period which means the anesthetic is working well.
We can see that during application time DPVA create more pain
than the LB (Figure 9).
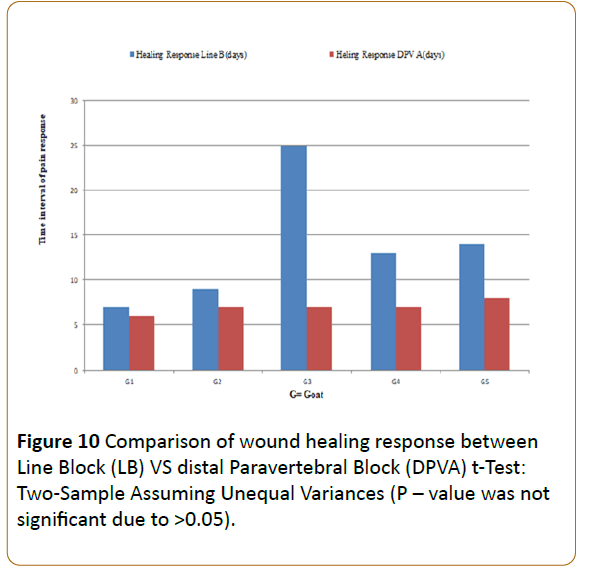
Comparison of wound healing response
Comparison between two techniques of wound healing
revealed that DPVA had good wound healing response than the
LB and there was no infection in DPVA but one case (Goat-3) had
a complication during the healing process which delayed the
time of healing (Figure 10).
Figure 10: Comparison of wound healing response between
Line Block (LB) VS distal Paravertebral Block (DPVA) t-Test:
Two-Sample Assuming Unequal Variances (P – value was not
significant due to >0.05).
Hematology parameter
The hematological values observed in this study were within
the normal range as the lignocaine had worked well to control
cardiac arrhythmia and suppressing automaticity and this may
have helped to keep the hematological parameters within a
normal range (Table 4).
| |
Mean scores |
| Parameters |
Groups |
Before surgery |
24 hours of surgery |
One week after surgery |
| RBC (× 106/l) |
DPVA |
12.32 ± 1.35 |
12.79 ± 1.23 |
12.23 ± 1.32 |
| MIA |
13.13 ± 0.51 |
13.69 ± 0.52 |
13.36 ± 0.85 |
| PCV (%) |
DPVA |
21.92 ± 2.56 |
24.66 ± 5.24 |
16.15 ± 2.85 |
| MIA |
25.22 ± 1.19 |
25.90 ± 1.15 |
25.72 ± 4.37 |
| Hemoglobin (g/d) |
DPVA |
8.12 ± 1.36 |
8.98 ± 2.25 |
8.63 ± 1.51 |
| MIA |
9.16 ± 0.43 |
9.84 ± 0.59 |
9.86 ± 1.28 |
| Total WBC (× 103/l) |
DPVA |
25.48 ± 4.19 |
37.70 ± 3.90 |
34.93 ± 3.12 |
| MIA |
33.86 ± 9.96 |
50.52 ± 16.32 |
51.08 ± 5.07 |
| Granulocytes (× 103/l) |
DPVA |
11.10 ± 3.69 |
13.24 ± 3.45 |
10.23 ± 5.72 |
| MIA |
11.38 ± 4.41 |
20.90 ± 10.51 |
18.62 ± 5.07 |
| Lymphocytes (× 103/l) |
DPVA |
11.74 ± 3.27 |
19.16 ± 2.61 |
21.33 ± 8.22 |
| MIA |
33.86 ± 3.40 |
24.06 ± 7.37 |
28.32 ± 11.98 |
| Monocytes (× 103/l) |
DPVA |
2.60 ± 0.89 |
4.08 ± 1.21 |
3.35 ± 0.66 |
| MIA |
4.14 ± 1.02 |
5.60 ± 1.54 |
4.12 ± 0.44 |
Table 4 Total leucocytes and differential leucocytes count before and after surgery of the DPVA and LB approaches (mean ± SD).
Discussion
Till date, the study reported here was the first in which
investigators compared two local anesthetic techniques for
laparotomy in the goats. 10 goats experiencing laparotomy were
divided into two groups where five animals, undertook a
technique consisting of an incisional line block and the other five
undertook distal paravertebral anesthesia. Both techniques
required a mean of five minutes to complete but the line block
method was considered more difficult than the distal
paravertebral anesthesia. After distal paravertebral anesthesia,
pain reactions to incision of the external oblique abdominal
muscle were more severe, however, reactions to abdominal
exploration and to suture the two oblique abdominal muscles
were significantly milder than after line block. Wound healing
was significantly better than inline block. Neither technique
resulted in a consistent and complete elimination of pain
reactions in every patient, but overall distal paravertebral
anesthesia had better results than the line block.
The assessment of the pain behavior of an animal is selfsame
life-threatening to measure in animals like cattle and goat [9,19].
About their specific pain expressions or the individual pain,
sensitivity is little known [19,20]. The administration of 6 ml
(100 mg) @ of 6 mg/kg BW of 2% lignocaine hydrochloride to
accomplish distal paravertebral nerve block produced
appreciable analgesia of the lateral abdominal wall. It is
noteworthy that 2 ml (40 mg) of the drug was deposited at each
site rather than 3 ml (60 mg) as specified by some authors. This
deliberate reduction in the volume of lignocaine has a significant
implication on both the economy of cost and reduced toxicity to
the animal, which supports my present study [7,26]. In the
course of the investigation, it became clear that not only the
comparison of the two methods but also the effectiveness of
local anesthesia was put to the test. The results obtained in this
study shown that the DPVA is more feasible and easier, which
was also recommended by Nuss [2]. The implementation of LB
not only referred to the inexperienced, but also more than 50%
of experienced anesthetists mention that as "not easy". Reason
for that it often deep or small hunger pit, worrying to hurt
abdominal organs, as well defensive movements of the animals.
Probably also played one role that the injection for the LB
because of the larger length also had a larger diameter than
those for the DPVA which was also recommended by Nuss [2].
For infiltration anesthesia should, therefore, be possible to use
thin needles to help the pain in the present examination could
about pain reactions. DPVA is less panic then the LB which is also
recommended by Nuss [2].
The present investigation was in the prospect of a better
distribution of the anesthetic and thereby achieve a better
effect. However, the DPVA was not in most cases as a mention
for [3,10] reliable in pain elimination. Furthermore, it would be
desirable to have more potent local anesthesia [3] for livestock
available, for longer operations. The BCS of the animals
influenced neither feasibility in the present study still the
effectiveness of anesthesia. In bleeding, the needle was
withdrawn and placed differently. Diffusion of the local
anesthetic toward the pelvic limb, recognizable by an unstable
state or by a decline of the Patients [7,23] could not be observed in any of the animals. For the assessment of pain during the
operation appeared the distinction in "no reaction", "unspecific
reaction" and "specific response" most important because the
pain cannot be eliminated. These findings encourage to refine
the anesthesia techniques and to use more advanced measures,
such as light sedation which is also recommended by Nuss et al.
[2].
Subcutaneous and muscular infiltration at LB provided good
anesthesia. At the incision of the Marcus obliquus externus
significantly underperformed the DPVA and LB obviously, the
local anesthetic was at the incision initially effective under LB in
the area of the cutting line and then quickly became non-specific
in the well-perfused muscle, which is recommended by Löscher
[24]. When wound closure was done, the effect got subsided, so
that the Marcus obliquus externus and internally abdominis
significantly showed more reactions after DPVA occurred. The
duration of action of lidocaine was thus too short for pain
response.
The present study reveals that the use of plain lidocaine
which is better than the combined with epinephrine which is
also recommended by Skarda et al. [3]. Study on DPVA, the
depth was in the nerve surrounding connective and fatty tissue,
thus reducing the active ingredient runs slower and the effect is
guaranteed longer which was also recommended by Link and
Smith [25]. At the LB were because of the rapid decay of the
effect also no differences in the painfulness at long continuous
and short-lasting operations determine. Therefore, for the
laparotomy in goats, a more potent local the anesthetic will be
available regarding the more difficult to infiltrate deeper muscle
layers. There were no differences between LB and DPVA in terms
of effectiveness. That's good, contrary to expectations cutting
off the LB in the deep layers are likely to be on their component,
which is believed to be one the DPVA equivalent anesthesia of
the inner layers contributed. Present study mention that
exploration of the abdominal cavity by local anesthetics
techniques among the DPVA significantly fewer signs of pain,
which is also recommended by Nuss [2]. During the study
period, replenishment was usually only after incision of the
external oblique abdominal, it is seen that the pain reactions
remained too strong. In the present Investigation when the
animals feel more pain then surgery pause for a while. This was
also practiced in other studies [26,27]. Sedation of the goat in
laparotomy is discussed in the literature. In recent years,
however, the opinions prevail, that the positive effects justify
the use of xylazine [14,23]. The Sedation is the mode of
administration of xylazine important. The intravenous
administration leads to a faster, more intensive effect and to
better analgesia than intramuscular administration. At the
subcutaneous injection is the least risk that the Animal goes
down [28]. but in the present research, there is no use of
xylazine for sedation. In the present study, there were slight
variations of total white blood cells (WBC) count of the two
approaches before surgery, at 24 hours, and at the first week
after surgery, the LB group had slight variation WBC value at all
the intervals with non-significant differences at first and second
week after surgery [29,30]. There were slight variations of total
granulocytes between the two groups with the LB group having
slightly higher values at all the intervals, but there is no significant difference between the two groups. The lymphocytes
values of the two groups also varied and the LB approach had
the slight highest value which is also supported by Abubakar
[18].
In present study seen that LB techniques for laparotomy
among five, one goat has shown edema in incision line and
wound healing delayed for 25 days but there is no any infection
seen in DPVA and wound healing seen in nearly 7-8 days but in
LB takes longer time then DPVA so we can say that DPVA is
better than the LB supported by Skarda [12].
In summary, it should be noted that both investigated
anesthesia techniques in a part of the animals are not
satisfactory pain switch was achieved. This unsatisfactory
effectiveness can be due to the technical implementation of
anesthesia, but also at the relatively weak effect and short
duration of action of lidocaine falsehood [31-35].
Conclusions
After conducting the study on comparison of two methods of
local anesthesia for laparotomy in goat had reached few
decisions like:
• Local anesthesia is very effective in field condition to save the
animals
• Both anesthetic techniques could reduce the pain completely
suppress reactions in only 50% of the animals.
• The pain was more reliably switched off under DPVA than
under MIA.
• A replenishment of local anesthetic should be scheduled for
both techniques become furthermore, slight sedation of the
animals which help to reduce more painless laparotomy.
• More potent local anesthetics as procaine 2%, for example,
lidocaine, should be used for the laparotomy in goat.
Acknowledgment
We would like to thank full to the directors of Shahidul Alam
Quadery Teaching Veterinary Hospital (SAQTVH).
References
- Hendrickson DA (2007) Techniques in Large Animal Surgery. Black, well Publishing, Ames, Iowa USA, 3rd edn, pp: 221-223.
- Nuss K, Eiberle BJ, Louis SC (2012) Comparison of two methods of local anaesthesia for laparotomy in cattle. Veterinary Practice 40: 141-149.
- Skarda RT, Tranquilli WJ (2007) Local and regional anesthetic and analgesic techniques: ruminants and swine. Lumb & Jones Veterinary Anesthesia and Analgesia, pp: 643-681.
- Taylor PM (1991) Anaesthesia in sheep and goats. Practice 1: 31-36.
- Smith MC, Sherman DM (2009) Dehorning and descenting. Goat Medicine, 2nd edn. pp: 723-731.
- Arnold JP, Kitchell RL (1957) Experimental Studies of the Innervation of the Abdominal Wall of Cattle. American Journal of Veterinary Research 67: 229-240.
- Ivany JM, Muir WW (2004) Farm animal anesthesia. Farm animal surgery. St Louis (MO): WB Saunders, pp: 97-112.
- Edmondson MA (2008) Local and regional anesthesia in cattle. Veterinary Clinics of North America: Food Animal Practice 24: 211-226.
- Steiner A, von-Rotz A (2003) The most important local anesthesia in cattle: A Review. Schweiz Arch Tierheilkd 145: 621-663.
- Farquharson J (1940) Paravertebral lumbar anesthesia in the bovine species. Journal of American Veterinary Medicine Association 1: 54-57.
- Ames NK (2007) Noordsy's. Food Animal Surgery. Wiley-Blackwell, 5th edn, p: 960.
- Skarda RT (1986) Techniques of local anesthesia in ruminants and swine. Veterinary Clinic North American Food Animal Practics 2: 621-663.
- Freeman DE (2003) Abdominal Surgery. Summary Procedure and Principles, International Veterinary Information Service, New York, USA, p: 22.
- Tuagi RP, Singh J (1993) Ruminant surgery. Textbook of the Surgical Disease of Cattle, Buffaloes, Camels, Sheep and Goats, C.S.B Publishers and Distributors, New Delhi, India 1: 195-223.
- Sylvestre A, Wilson J, Hare J (2002) A comparison of two different suture patterns for skin closure of canine ovariohysterectomy. The Canadian Veterinary Journal 43: 699-702.
- Egbe-Niyi TN, Nwaosu SC, Salami HA (2000) Haematology values of apparently healthy sheep and goats as influenced by age and sex in arid zone of Nigeria. African Journal of Biomed Research 1: 109-115.
- Egbe-Niyi TN, Nwaosu SC, Salami HA (2000) Haematology values of apparently healthy sheep and goats as influenced by age and sex in arid zone of Nigeria. African Journal of Biomed Research, pp: 109-115.
- Abubakar AA, Andeshi RA, Yakubu AS, Lawal FM, Adamu U (2014) Comparative Evaluation of Midventral and Flank Laparotomy Approaches in Goat. Journal of Veterinary Medicine, p: 6.
- Feist M, Köstlin R, Nuss K (2008) Examination of the Pain Expression Behavior of Cows after Claw Surgery. Veterinarian Practice 36: 367-376.
- Anderson DE, Muir WW (2005) Pain management in ruminants. Veterinary Clinics. Food Animal Practice, pp: 19-31.
- Olaifa AK, Olatunji-Akioye AO, Agbaje LO, Olatunji-Akioye AO (2009) Distal paravertebral nerve block effects on west african dwarf goat hematology and physiology. Israel Journal of Veterinary Medicine, p: 128.
- Clarke KW, Trim CM (2013) Veterinary Anaesthesia E-Book. Elsevier Health Sciences, p: 352.
- Muir MW, Hubbell JA, Bednarski RM, Skarda RT (2005) Local anesthesia in ruminants and pigs. Handbook of Veterinary Anesthesia (4th edn) Mosby, St. Louis, USA, pp: 72-99.
- Löscher W (2006) Local anesthetics. Pharmacotherapy for domestic animals and livestock. 7th Parey in MVS Medical Publishing, pp: 125-130.
- Link RP, Smith JCZ (1956) Comparison of some local anesthetics in cattle. Journal of the American Veterinary Medical Association 129: 306-309.
- Holton L, Reid J, Scott EM, Pawson P, Nolan A (2001) Development of a behavior-based scale to measure acute pain in dogs. Veterinary Record 1: 525-531.
- Underwood WJ (2002) Pain and distress in agricultural animals. Journal of American Veterinary Medicine Association 221: 208-211.
- Budras KD, Wünsche A (2002) Atlas of the anatomy of the bovine. Hannover, Schlütersche GmbH and Co. KG, Publishing and Printing.
- Dietz O, Henschel E, Busch W (1988) Anesthesia and operations on large and small animals. Sink, p: 215.
- Frey HH, Löscher W (2002) Textbook of pharmacology and toxicology for veterinary medicine. Sink, p: 364.
- Henke J, Erhardt W, Tacke S (2008) Analgesic protocols before, during and after anaesthesia of dogs and cats in painful situations. Veterinary Practice of Small Animals/pets 36: 27-34.
- Hudson CD, Whay HR, Huxley JN (2008) Recognition and management of pain in cattle. In Practice/BJM Journals 30: 126-134.
- Nickel R, Schummer A, Seiferle E (1992) Textbook of the Anatomy of Pets, Musculoskeletal System. Berlin and Hamburg Parey, p: 256.
- Nuss K, Eiberle BJ, Louis SC (2012) Comparison of two local anesthetic techniques for laparotomy in cattle. Veterinary Practice G: Large Animals/Livestock 40: 141-149.
- Callaghan KO (2002) Lameness in cattle and associated pain in cattle. Challenging Traditional Perceptions, pp: 212-219.